TEFCA and the Promise of Nationwide Healthcare Interoperability: Beyond Treatment to a True National Health Data Network
Introduction
On a cold January morning in 2024, the first official messages began flowing across America's newest health information superhighway. After years of planning, development, and anticipation, the Trusted Exchange Framework and Common Agreement—TEFCA—had finally gone live. Healthcare organizations across the country could now exchange patient information through newly designated Qualified Health Information Networks, creating the foundation for what many hoped would become a seamless nationwide health data utility.
This milestone represented both an achievement and a beginning. For the Office of the National Coordinator for Health Information Technology (ONC) and the healthcare interoperability community, TEFCA's launch marked the culmination of a journey that began with the 21st Century Cures Act in 2016. But for the broader healthcare ecosystem—providers, payers, technology vendors, public health authorities, researchers, and patients—it marked the start of a new chapter in America's long and often frustrating quest for healthcare interoperability.
Now, over a year into TEFCA's operational phase, a critical question emerges: Will this ambitious framework fulfill its broader promise, or will it remain primarily focused on clinical data exchange between healthcare providers? The question matters deeply because TEFCA was explicitly designed to support multiple exchange purposes beyond treatment: payment, healthcare operations, individual access, public health, government benefits determination, and research. Yet progress on these additional exchange purposes has lagged significantly behind the core treatment use case.
This divergence between TEFCA's comprehensive vision and its more limited initial implementation reflects deeper patterns in healthcare interoperability. Throughout its history, American healthcare has made more progress on clinical data exchange for direct patient care than on sharing data for other purposes. The pattern persists despite widespread recognition that comprehensive interoperability—spanning clinical and administrative domains, supporting diverse stakeholders, and enabling multiple data uses—is essential for transforming healthcare delivery, improving efficiency, and empowering patients.
The healthcare ecosystem now stands at a critical juncture. Will TEFCA follow the path of previous interoperability initiatives that started with grand visions but ultimately delivered more limited results? Or will it evolve into the comprehensive national health data utility envisioned by its architects? The answer depends on how effectively the ecosystem navigates the complex technical, operational, economic, and policy challenges that have historically constrained interoperability efforts.
This essay explores TEFCA's potential to transcend its current limitations and create a truly comprehensive nationwide health information network. It examines the historical context that shaped TEFCA's development, analyzes the current state of implementation, identifies the key forces influencing its trajectory, and presents a vision for how TEFCA might evolve to fulfill its broader promise. Throughout, it considers the perspectives of diverse stakeholders and the strategies that might enable progress toward comprehensive interoperability that serves the entire healthcare ecosystem.
The Journey to TEFCA: Learning from History
To understand TEFCA's potential and challenges, we must first understand the historical context from which it emerged. America's quest for healthcare interoperability has unfolded over more than two decades, with recurring patterns of ambition, investment, progress, and limitation that continue to shape current efforts.
In the early 2000s, healthcare remained largely paper-based, with electronic health records (EHRs) present in only a small minority of hospitals and physician practices. President George W. Bush established the Office of the National Coordinator for Health Information Technology in 2004 and set an ambitious goal: most Americans would have electronic health records by 2014. The vision extended beyond mere digitization to include the seamless exchange of health information across organizational boundaries.
"Information should follow the patient, and artificial organizational boundaries should not be a barrier to the seamless delivery of health care," declared David Brailer, the first National Coordinator, articulating a vision that would guide interoperability efforts for years to come. Early initiatives focused on developing standards, creating regional health information organizations, and establishing a nationwide health information network that would connect these regional exchanges.
The HITECH Act of 2009 dramatically accelerated healthcare's digital transformation, providing nearly $30 billion to promote EHR adoption through the Meaningful Use program. Within a decade, EHR adoption rose from less than 10% to over 90% of hospitals and nearly 80% of physician practices. However, this rapid digitization occurred without sufficient attention to interoperability, creating what some observers called "digital islands" of information rather than a connected ecosystem.
"We've digitized the tower of Babel," lamented one health system CIO during this period, capturing the frustration of finding that even with widespread EHR adoption, information remained stubbornly siloed. The Meaningful Use program did include interoperability requirements, but these focused primarily on basic exchange capabilities rather than comprehensive data sharing across the healthcare ecosystem.
The early 2010s saw significant growth in health information exchanges (HIEs) at state and regional levels, alongside private networks like Epic's Care Everywhere, CommonWell, Carequality, and eHealth Exchange. These networks made impressive progress in enabling provider-to-provider exchange for treatment purposes, but remained fragmented and incomplete. Cross-network exchange remained challenging, participation was voluntary, and many organizations remained outside these networks altogether.
Furthermore, these networks primarily focused on provider-to-provider exchange for treatment purposes, with limited support for other exchange purposes like payment, operations, or individual access. This focus reflected both technical realities—the predominant exchange standards were designed primarily for clinical document exchange—and market dynamics, as providers saw clearer value in clinical data exchange than in sharing information for other purposes.
By the mid-2010s, frustration with the pace of interoperability progress had grown among policymakers, patient advocates, and many healthcare leaders. The 21st Century Cures Act, passed with bipartisan support in 2016, aimed to address these limitations through several interoperability provisions:
It mandated that ONC develop a Trusted Exchange Framework and Common Agreement to establish a nationwide floor of interoperability across disparate networks.
It prohibited information blocking—practices that unreasonably interfere with the exchange or use of electronic health information.
It required standardized application programming interfaces (APIs) that would enable individuals to access their health information using smartphone applications.
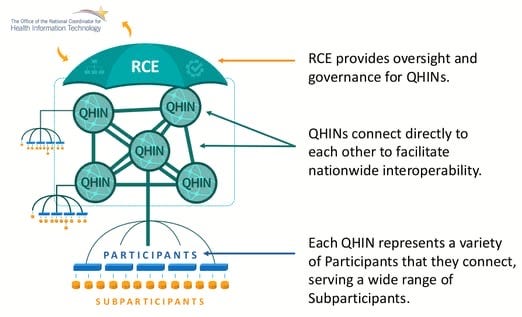
TEFCA emerged from this legislative mandate as a framework designed to bridge existing networks, establish universal interoperability, and support diverse exchange purposes beyond treatment. After years of development, including multiple rounds of public comment, TEFCA was finally published in 2022, with The Sequoia Project designated as the Recognized Coordinating Entity (RCE) responsible for implementing and governing the framework.
The first QHINs—CommonWell Health Alliance, eHealth Exchange, Epic Interoperability Exchange, Health Gorilla, Kno2, and KONZA—were designated in 2023, and live exchanges began in early 2024. This timeline—eight years from legislation to implementation—highlights one persistent pattern in healthcare interoperability: progress consistently takes longer than initially projected.
Other historical patterns also continue to influence TEFCA's evolution. Policy interventions have been essential catalysts for progress but have often struggled to overcome entrenched market dynamics. Technical standards and capabilities have advanced more rapidly than organizational readiness and financial incentives to share data. And despite broad rhetorical commitment to comprehensive interoperability, actual implementation has typically focused first on clinical data exchange for treatment purposes, with other exchange purposes developing more slowly.
As TEFCA continues to evolve, these historical patterns suggest both caution and opportunity. The caution lies in recognizing that previous interoperability initiatives have often delivered less than initially promised, particularly for exchange purposes beyond clinical care. The opportunity lies in learning from this history to develop more effective strategies for overcoming the persistent barriers to comprehensive interoperability.
TEFCA Today: Progress and Limitations
After more than a year of operational exchange, TEFCA has established a functional foundation for nationwide health information exchange but remains limited in several key respects. The six designated QHINs have built the basic technical infrastructure for nationwide exchange, connected significant numbers of participants, and begun to facilitate actual data exchange. However, network effects remain nascent, participation is uneven across the healthcare ecosystem, and several exchange purposes remain more theoretical than practical.
Maria Rodriguez, Chief Information Officer at a mid-sized health system in the Midwest, describes her organization's experience with TEFCA: "We joined through our existing HIE relationship, and we're definitely seeing benefits for clinical exchange. When patients come in from other regions, we're more likely to find their records now. But it's still focused on the basics—getting clinical documents when we need them for patient care. All the other potential uses of TEFCA are still on the horizon for us."
This experience reflects the broader reality of TEFCA implementation. Progress has been most notable for treatment-related exchange between providers, with capabilities for finding and retrieving clinical documents about patients from other organizations. This focus is understandable for several reasons. Treatment exchange builds directly on the capabilities and policies that QHINs and their participants had already developed through their pre-TEFCA networks. Additionally, treatment exchange faces fewer policy and operational barriers than other exchange purposes, as the HIPAA treatment permission provides a clear legal basis for sharing, and workflows for incorporating external clinical data into care delivery are relatively well-established.
In contrast, progress on other exchange purposes—payment, healthcare operations, individual access, public health, government benefits, and research—has been markedly slower. The TEFCA Common Agreement and Standard Operating Procedures (SOPs) establish the basic legal and policy framework for these exchange purposes, but implementation has been hampered by various factors.
For payment-related exchange, payer participation in QHINs remains limited, and the technical framework hasn't been fully adapted to support payment-specific use cases. "We're watching TEFCA with interest," says Thomas Chen, Vice President for Data Strategy at a national health insurance company, "but right now, we're getting the clinical data we need through direct connections with provider organizations and our existing data aggregation partners. The value proposition for joining a QHIN isn't clear enough yet for us to make that investment."
For healthcare operations, the challenge involves both definition and implementation. "Operations covers such a wide range of activities," explains Samantha Washington, Director of Data Governance at a large academic medical center. "Quality measurement, population health management, utilization review—each has different data needs and stakeholders. TEFCA gives us the legal framework to exchange for these purposes, but the technical and operational details still need to be worked out for most operations use cases."
Individual access through TEFCA remains particularly underdeveloped. While the Common Agreement includes individual access as a permitted exchange purpose, few QHINs have implemented robust consumer-facing capabilities. "The challenge isn't just technical," says Michael Johnson, CEO of a patient advocacy organization. "It's about creating an ecosystem where individuals can easily discover, access, and use their health information from multiple sources. That requires not just exchange capabilities but user-friendly interfaces, identity verification processes, and educational resources to help people make sense of their data."
Public health, government benefits, and research exchange face similar implementation gaps. While these exchange purposes are permitted under TEFCA, the practical mechanisms for facilitating them remain limited. Government agencies, public health authorities, and research organizations have had less involvement in TEFCA development and implementation compared to healthcare providers and health IT vendors, contributing to slower progress in these areas.
This uneven implementation across exchange purposes reflects both practical prioritization decisions and deeper structural challenges. The RCE and QHINs adopted a phased approach, focusing first on establishing basic exchange capabilities for treatment before expanding to other purposes. This approach makes sense given limited resources and the complexity of the overall undertaking. However, it also risks reinforcing the historical pattern of prioritizing treatment exchange over other purposes, potentially limiting TEFCA's broader impact.
The current state of TEFCA implementation also reveals several cross-cutting challenges that affect all exchange purposes:
Network effects remain nascent. While the six QHINs provide theoretical coverage for a significant portion of the healthcare ecosystem, many organizations remain outside the TEFCA network, limiting its reach and utility.
Technical capabilities are still evolving. The initial TEFCA technical framework, built around document-centric exchange, has limitations for supporting diverse exchange purposes that might benefit from more granular, API-based exchange patterns.
Governance structures are maturing. The multi-layered governance model—spanning federal oversight, RCE governance, QHIN governance, and participant governance—creates complexity that can be challenging to navigate, particularly for smaller organizations or those new to health information exchange.
Economic models remain in development. The long-term financial sustainability of TEFCA depends on developing viable business models at multiple levels, from federal funding to QHIN operations to participant investments, and these models are still evolving.
Despite these limitations, the current state of TEFCA represents significant progress compared to the fragmented exchange landscape that preceded it. The framework has established a legal and technical foundation for nationwide exchange that can potentially support all the envisioned exchange purposes. The challenge now is to build on this foundation to create a truly comprehensive network that serves the full range of stakeholders and use cases.
Beyond Treatment: The Potential of Comprehensive Exchange
To understand TEFCA's full potential, we must look beyond its current implementation to examine what comprehensive interoperability across all exchange purposes might enable. Each exchange purpose offers distinct value propositions for different stakeholders and faces unique implementation challenges.
Payment: Bridging Clinical and Financial Worlds
Payment-related exchange involves sharing health information to support activities like claims processing, prior authorization, risk adjustment, and utilization management. This exchange purpose has significant potential to reduce administrative costs, improve payment accuracy, and reduce provider burden.
"The administrative costs in healthcare are staggering," notes Dr. Robert Anderson, Chief Medical Officer at a regional physician network. "My physicians spend hours every week dealing with prior authorizations, documenting for risk adjustment, responding to payer audits—all activities that could be streamlined with better data exchange. If TEFCA could help address these pain points, that would be transformative."
The potential benefits of payment-related exchange through TEFCA are substantial:
For providers, streamlined prior authorization could reduce administrative burdens, decrease care delays, and improve patient satisfaction. More efficient claims processing could improve revenue cycle performance and reduce the costs of managing denials and appeals. And automated quality reporting could reduce the burden of documenting for value-based payment programs.
For payers, more comprehensive clinical data access could improve risk adjustment accuracy, enhance care management programs, and reduce the need for costly manual record reviews. Better data exchange could also support more sophisticated payment models that align financial incentives with quality and outcomes.
For patients, improved payment-related exchange could mean fewer delays in receiving needed care, reduced administrative hassles, and potentially lower costs as administrative savings are passed through to premiums and out-of-pocket expenses.
Despite these potential benefits, payment-related exchange through TEFCA faces significant implementation challenges. Clinical and financial data systems have historically been separate, with distinct standards, workflows, and stakeholders. Payer participation in QHINs remains limited, as many insurers have invested in their own data acquisition strategies. And the trust relationships between providers and payers are often complex, with some providers hesitant to share data that might be used for payment denials or audits.
"There's a fundamental trust issue that needs to be addressed," explains Sarah Martinez, Vice President for Provider Relations at a Blue Cross Blue Shield plan. "Providers worry that easier access to clinical data will just lead to more denials and audits. We need to demonstrate that better data exchange can actually reduce administrative burden and support more collaborative relationships focused on value and outcomes."
For TEFCA to successfully support payment-related exchange, several developments will be necessary. Major payers must join QHINs, either directly or through intermediaries, to create network effects. The TEFCA technical framework may need to incorporate additional standards specifically designed for payer-provider exchange, such as FHIR-based Da Vinci implementation guides. Governance mechanisms must address the unique considerations of payment-related exchange to build provider confidence. And implementation efforts should align with other interoperability initiatives focused on payment, such as the CMS Interoperability and Prior Authorization Rule.
Progress will likely be incremental, beginning with specific use cases where benefits are clear and incentives are aligned, such as prior authorization or risk adjustment data exchange. With continued policy support and market evolution, payment exchange through TEFCA could eventually become routine, but this transition will likely require several years of steady development.
Healthcare Operations: Enhancing System Performance
Healthcare operations encompasses a diverse range of activities, including quality assessment and improvement, population health management, care coordination beyond immediate treatment, credentialing, and business planning. This exchange purpose spans both clinical and administrative domains and involves various stakeholders, including providers, payers, quality organizations, and health IT vendors.
"Operations is where a lot of the real transformation in healthcare happens," observes Dr. James Wilson, Chief Quality Officer at an integrated delivery network. "It's not just about treating individual patients but about making the system work better as a whole. That requires looking at patterns across populations, measuring and improving performance, coordinating care across teams and settings. All of that depends on having good data that crosses organizational boundaries."
The potential benefits of operations-related exchange through TEFCA are significant:
For healthcare organizations, more comprehensive data access could enhance quality improvement initiatives, strengthen population health management programs, improve care coordination for complex patients, and support more effective resource allocation and planning.
For patients, improved operations-related exchange could lead to better-coordinated care, reduced gaps in care, and higher-quality healthcare services overall.
For the healthcare system as a whole, better operations-related exchange could accelerate performance improvement, reduce waste and duplication, and support the transition to more integrated, value-based care models.
Despite these potential benefits, operations-related exchange through TEFCA faces implementation challenges. The broad definition of "healthcare operations" encompasses numerous distinct activities with different data needs, stakeholder involvement, and sensitivity levels. Organizations interpret HIPAA's operations provisions differently, creating uncertainty about when data can be shared without additional authorization. And unlike treatment exchange, where benefits are relatively clear, the value proposition for operations exchange varies widely depending on the specific use case and organizational context.
"One of the challenges is that operations use cases often require different data than what's typically exchanged for treatment," explains David Thompson, Director of Data Analytics at a state-level HIE. "Instead of documents about specific patients, you might need structured data elements for entire populations, historical trends over time, or specialized metrics that aren't routinely captured in clinical documents. The technical framework needs to evolve to support these different exchange patterns."
For TEFCA to effectively support operations-related exchange, several developments will be necessary. The RCE and stakeholders need to develop more detailed specifications for specific operations use cases, clarifying data requirements, exchange patterns, and policy considerations. QHINs may need to develop additional capabilities beyond those required for treatment exchange, such as bulk data exchange, advanced query parameters, and analytics support. And governance frameworks must evolve to address new considerations around appropriate use, audit, and oversight.
Progress on operations-related exchange will likely follow a pattern of incremental expansion, beginning with specific use cases that have clear value propositions and straightforward policy considerations, such as quality measurement, care coordination, or credentialing. Over time, as experience grows and technical capabilities mature, the scope of operations exchange may expand to encompass more complex use cases.
Individual Access: Empowering Patients as Data Stewards
Individual access involves enabling patients to access, obtain, and direct the sharing of their own health information. This exchange purpose is distinct from others in that it places the individual, rather than a covered entity, at the center of the exchange relationship.
"Patients should be more than passive recipients of care," argues Lisa Chen, a patient advocate and cancer survivor. "We should be active participants in our health journeys, with the ability to access our complete health information, understand it, and share it as needed. Right now, getting my health data is still too fragmented and difficult. I have different patient portals for different providers, each with partial information. A truly national system that gives me access to all my health information would be transformative."
The potential benefits of individual access through TEFCA are substantial:
For patients, comprehensive access to their health information could enhance their ability to manage their health, coordinate their own care across providers, detect errors in their records, and make more informed decisions. The ability to direct the sharing of their information with third-party applications or services could enable new tools and services that help them understand and use their health data more effectively.
For providers, patient-directed exchange could reduce the burden of managing record requests, facilitate access to patient-generated health data, and support more collaborative relationships with patients.
For innovators, standardized patient-directed access to health information could enable new applications and services that help patients manage their health, potentially creating new markets and business models.
Despite these potential benefits, individual access through TEFCA faces significant implementation challenges. Enabling individual access requires additional technical capabilities beyond provider-to-provider exchange, including consumer authentication, authorization management, and user-friendly interfaces. Establishing reliable methods to verify individuals' identities while maintaining accessibility presents significant challenges. And sustainable business models for individual access services remain unclear, particularly regarding who pays for the infrastructure and services.
"The technical challenge is only part of the picture," notes Michael Torres, CEO of a health technology startup focused on consumer applications. "We also need to solve the usability challenge—making it easy for people with different levels of technical and health literacy to find, access, and use their health information. And we need sustainable economic models that support the infrastructure required for individual access without creating financial barriers for patients."
For TEFCA to successfully support individual access, several developments will be necessary. QHINs will need to develop or partner with entities that provide consumer-facing portals, authentication services, and consent management tools. Robust yet accessible identity proofing and authentication solutions must be implemented to balance security with usability. Technical requirements must align with emerging standards for consumer-directed exchange, such as SMART on FHIR and UMA (User-Managed Access). And sustainable business models for individual access services must emerge, potentially involving contributions from various stakeholders.
Progress on individual access through TEFCA will likely involve both direct and indirect approaches. Some QHINs may develop their own consumer-facing services, while others may partner with existing consumer platforms or enable their participants to offer individual access through their own patient portals. Over time, as these approaches mature and converge, individual access could become a core component of the TEFCA ecosystem.
Government Benefits, Public Health, and Research: Serving Broader Public Interests
Beyond the healthcare delivery system, TEFCA was designed to support exchange purposes that serve broader public interests, including government benefits determination, public health, and research. These exchange purposes involve different stakeholders, legal frameworks, and technical requirements than provider-focused exchange.
"The COVID-19 pandemic highlighted both the critical importance of public health data exchange and the significant gaps in our current capabilities," observes Dr. Jennifer Lewis, an epidemiologist at a state health department. "We struggled to get comprehensive, timely data on cases, hospitalizations, and outcomes. A robust national infrastructure that connects clinical data systems with public health could dramatically enhance our ability to monitor and respond to health threats."
Similarly, research and government benefits determination could be significantly enhanced by more comprehensive data exchange. Clinical researchers often struggle to access representative patient data across organizations, limiting their ability to address important research questions. And determining eligibility for government programs like disability benefits often involves lengthy, paper-based processes for obtaining medical documentation.
The potential benefits of these broader exchange purposes through TEFCA are substantial:
For public health authorities, more comprehensive and timely access to clinical data could enhance disease surveillance, outbreak detection, population health monitoring, and program evaluation. Rather than relying on fragmented, often delayed reporting systems, public health agencies could have more complete, near-real-time visibility into health patterns and trends.
For researchers, standardized access to diverse clinical data sources could accelerate discoveries, enhance trial recruitment, improve representativeness of study populations, and enable more robust health services research. TEFCA could potentially serve as a foundation for a learning health system that systematically generates and applies evidence to improve care.
For government agencies, streamlined access to clinical documentation could improve the efficiency and accuracy of benefits determination processes, reducing delays for beneficiaries and administrative costs for agencies.
For individuals, these broader exchange purposes could translate into better public health protection, more rapid medical advances, and more efficient government services.
Despite these potential benefits, implementation of these broader exchange purposes under TEFCA faces significant challenges. Government agencies, public health authorities, and research organizations have had limited involvement in TEFCA development and implementation. These exchange purposes often involve legal frameworks beyond HIPAA, creating additional complexity. And technical integration between TEFCA and the specialized systems used for public health, research, and government functions requires additional development work.
"There's also a resource challenge," notes Dr. Lewis. "Many public health agencies are chronically underfunded and still working with outdated technologies. Participating in a modern, API-based health information network requires investments in infrastructure, workforce, and operations that many agencies simply don't have the resources to make without dedicated funding."
For TEFCA to effectively support these broader exchange purposes, several developments will be necessary. Federal and state agencies must actively participate in TEFCA, either by joining QHINs themselves or establishing clear pathways for data exchange with their existing systems. TEFCA policies must align with agency-specific requirements, public health laws, and research regulations. Technical solutions must be developed to bridge TEFCA's exchange capabilities with specialized systems. And dedicated funding streams may be necessary to support the infrastructure and operations required.
Progress on these broader exchange purposes will likely be driven by specific initiatives and use cases. For example, targeted federal funding for particular public health use cases, specific research networks leveraging TEFCA infrastructure, or pilot programs for government benefits determination could serve as catalysts for expanding TEFCA's capabilities in these areas. Over time, as experience grows and technical solutions mature, more comprehensive approaches may emerge.
Navigating the Complexities: Key Challenges and Opportunities
Expanding TEFCA beyond treatment exchange involves navigating several complex domains that cut across all exchange purposes: legal and consent considerations, technical capabilities, economic models, and governance structures. Each domain presents both challenges and opportunities for advancing comprehensive interoperability.
Legal and Consent Frameworks: Balancing Exchange and Protection
One of the most significant challenges facing TEFCA's expansion is navigating the complex legal landscape of health information privacy and consent. While HIPAA provides a relatively clear framework for treatment-related exchange, other exchange purposes often involve additional legal considerations, varying interpretations, and more complex consent requirements.
"The legal landscape is like a patchwork quilt," observes Patricia Nguyen, Chief Privacy Officer at a multi-state health system. "We have HIPAA at the federal level, but then state laws that are often more stringent, especially for sensitive information like behavioral health, substance use disorder, or reproductive health. Then specific federal protections like 42 CFR Part 2 for substance use disorder records. Navigating all these requirements in a nationwide exchange network is extraordinarily complex."
The TEFCA Common Agreement and SOPs establish a basic framework for handling these considerations, but implementation reveals several key challenges. State privacy laws impose varying requirements beyond HIPAA, creating significant complexity for nationwide exchange. Different exchange purposes may require different consent models, from opt-out approaches for treatment to explicit authorization for certain operations or individual access scenarios. And questions about legal liability, breach responsibility, and enforcement across complex exchange networks create uncertainty that can inhibit participation.
"Trust is fundamental to health information exchange," explains Mark Johnson, General Counsel for a QHIN. "Organizations need clarity about their legal obligations and protections when participating in nationwide exchange. Without that clarity, many will take conservative approaches that limit data sharing even when it could benefit patients and the system."
Addressing these legal challenges requires a multi-faceted approach. Policy efforts to harmonize state privacy laws or establish federal preemption could reduce legal complexity, though such changes face significant political challenges. Advanced consent management technologies, including digital consent, granular permission models, and automated policy enforcement, can help manage complexity at scale. Clear, authoritative guidance from regulators regarding how various privacy laws apply in the TEFCA context could reduce uncertainty and facilitate participation. And TEFCA governance structures must continue to evolve to address emerging privacy considerations and establish clear responsibility frameworks.
Progress in this area will likely involve both technical and policy innovations. On the technical side, more sophisticated consent management capabilities, metadata tagging for sensitive information, and automated policy enforcement may emerge. On the policy side, efforts to clarify or harmonize legal requirements, establish consistent interpretation frameworks, and develop model policies for specific exchange scenarios will be important.
For potential TEFCA participants, especially those interested in exchange purposes beyond treatment, understanding and navigating this complex legal landscape represents a significant challenge. Organizations must assess their own risk tolerance, develop appropriate policies and procedures, and implement technical safeguards to ensure compliance while enabling appropriate exchange.
Technical Evolution: From Documents to Data
TEFCA's technical framework was initially built around document-centric exchange paradigms, reflecting the predominant standards and capabilities at the time of its development. However, the healthcare ecosystem is increasingly moving toward more granular, API-based data exchange, exemplified by the FHIR standard. This evolution has significant implications for TEFCA's potential to support comprehensive interoperability.
"Document exchange made sense as a starting point because it built on established standards and capabilities," explains Miguel Rodriguez, Chief Technology Officer at a health information exchange. "But many of the use cases beyond treatment exchange—particularly those involving individual access, payment processes, or analytics—benefit from more granular, structured data access rather than document retrieval. The technical framework needs to evolve to support these different exchange patterns."
The current TEFCA technical framework, known as QHIN Technical Framework (QTF), primarily supports document-centric query and message delivery, allowing participants to search for and retrieve clinical documents about a patient or send information to specific recipients. While these modalities provide a functional foundation for basic exchange, they have significant limitations for supporting the full range of exchange purposes and use cases envisioned for TEFCA.
Document-centric exchange makes it difficult to access specific data elements without retrieving and processing entire documents, creating inefficiencies for many use cases. Integrating document-based information into modern healthcare applications and workflows often requires additional processing and transformation steps. And the document paradigm can constrain innovation in healthcare applications and services that require more flexible, granular data access.
Recognizing these limitations, the ONC and RCE have signaled their intention to evolve the QTF to incorporate FHIR-based exchange. This evolution represents both an opportunity and a challenge for TEFCA. FHIR adoption could significantly expand TEFCA's utility for diverse exchange purposes, enable more efficient data integration, and align with broader industry trends toward API-based exchange. However, implementing FHIR at the QHIN level requires addressing complex considerations around scaling, security, patient matching, and governance that go beyond typical FHIR implementations.
"FHIR works well for direct connections between specific applications and data sources," notes Dr. Karen Chen, an interoperability specialist at a major health system. "But scaling it to nationwide exchange across thousands of organizations raises new challenges around discovery, routing, security, and performance. We need to thoughtfully address these challenges to realize FHIR's potential in the TEFCA context."
Several key technical developments will be necessary for TEFCA to achieve true data liquidity. The QTF must evolve to support FHIR-based exchange patterns, including both RESTful APIs and bulk data capabilities, while maintaining backward compatibility with document exchange. More robust identity management solutions will be essential for secure, reliable exchange. Technical approaches for scaling FHIR exchanges to nationwide volumes must be developed and implemented. And solutions for improving data quality, normalizing variations, and translating between different information models will be increasingly important as exchange volumes grow.
Progress in this area will likely follow an incremental path, with FHIR capabilities being added to the QTF over time while maintaining support for document exchange. This dual-track approach allows participants to adopt newer standards at their own pace while ensuring continuous interoperability.
For TEFCA to fulfill its potential as a comprehensive interoperability framework, this technical evolution is essential. Without support for more granular, API-based exchange patterns, TEFCA risks becoming increasingly misaligned with industry trends and unable to support the full range of exchange purposes it was designed to enable.
Economic Considerations: Sustainable Models for Comprehensive Exchange
Creating and sustaining a nationwide health information network requires substantial investments in infrastructure, operations, governance, and ongoing innovation. The economic model for TEFCA remains a work in progress, with significant questions about how to distribute costs and benefits across the ecosystem.
"The fundamental economic challenge is that the benefits of interoperability are often diffuse and accrue to different stakeholders than those bearing the costs," explains Dr. Michael Jefferson, a health economist studying interoperability investments. "A provider organization might invest in robust exchange capabilities, but the benefits might flow to patients, payers, or other providers. This misalignment of incentives has consistently slowed interoperability progress."
The current TEFCA economic model involves several layers. ONC has provided funding to the RCE to establish and operate the TEFCA framework, but this funding is limited in both amount and duration. QHINs must develop sustainable business models to cover their costs, which may include fees charged to participants, value-added services, or other revenue streams. And organizations that connect to QHINs must invest in their own technical capabilities, operational processes, and governance structures to participate effectively.
This multi-layered approach faces several challenges. The value of TEFCA participation depends significantly on network effects, creating chicken-and-egg problems in the early stages of implementation. Some organizations view health information as a competitive asset rather than a public good, creating resistance to sharing through open frameworks. And as federal seed funding diminishes, ensuring the long-term financial sustainability of the TEFCA ecosystem becomes increasingly challenging.
"We need to think of core health information exchange infrastructure as a public good, similar to roads or bridges," argues Sarah Williams, Executive Director of a state-level HIE. "It creates value for the entire healthcare ecosystem and society more broadly. That suggests we need sustainable public funding models alongside private investment, not just one-time grants or startup funding."
Addressing these economic challenges requires a multi-faceted approach. Clearer articulation of the specific value propositions for different stakeholders and exchange purposes can help build participation and willingness to invest. Policy interventions, including requirements, incentives, or payment models that reward interoperability, can help align economic incentives with broader system goals. QHINs and other participants must develop innovative business models that create sustainable revenue streams while promoting broad participation. And reconceptualizing core health information exchange infrastructure as a public good worthy of sustained public investment may be necessary for long-term sustainability.
The evolution of the TEFCA economic model will significantly influence which exchange purposes and use cases gain traction. Exchange patterns that offer clear, concentrated value to specific stakeholders may advance more rapidly than those with more diffuse benefits. Similarly, exchange purposes that align with existing revenue streams or regulatory requirements may see faster adoption than those requiring new business models.
For TEFCA to achieve its full potential as a comprehensive interoperability framework, its economic model must evolve to support diverse exchange purposes, ensure equitable access, and provide long-term sustainability. This evolution will require creativity, collaboration, and potentially new policy frameworks that recognize health information exchange as an essential component of healthcare infrastructure.
Governance Evolution: Managing a Complex Ecosystem
TEFCA establishes a complex governance framework spanning multiple levels, from federal oversight to QHIN operations to participant policies. This governance framework must balance multiple, sometimes competing objectives: ensuring trust and reliability, enabling innovation, protecting privacy, promoting participation, and supporting diverse exchange purposes.
"Effective governance is about creating the conditions for productive collaboration among diverse stakeholders," explains Dr. Robert Johnson, who serves on a QHIN governance committee. "It's about establishing clear rules of the road, processes for making decisions, mechanisms for accountability, and forums for addressing emerging issues. As TEFCA expands beyond basic treatment exchange, governance becomes even more critical because the stakeholders and use cases become more diverse."
The current TEFCA governance model includes several key components. ONC maintains ultimate authority over the TEFCA framework, setting high-level requirements and designating the RCE. The Sequoia Project, as the RCE, develops, maintains, and enforces the Common Agreement and SOPs, designates QHINs, and coordinates the overall TEFCA ecosystem. Each QHIN establishes its own governance structures for its participants, within the parameters
Each QHIN establishes its own governance structures for its participants, within the parameters established by the Common Agreement. And QHIN participants, including health systems, HIEs, and health IT vendors, maintain their own governance processes for their internal operations and connections.
This multi-layered governance model faces several challenges. The layered structure creates complexity that can be difficult for participants to navigate, particularly smaller organizations with limited resources. Balancing the need for consistent baseline requirements with flexibility to address diverse stakeholder needs creates ongoing tensions. Ensuring appropriate representation of diverse stakeholders, including those focused on non-treatment exchange purposes, presents ongoing challenges. And governance structures must evolve to address emerging technologies, use cases, and policy considerations without creating instability or excessive compliance burdens.
"One of our biggest governance challenges is adapting to new exchange purposes and use cases without having to reinvent the entire framework," notes Elizabeth Chen, a governance specialist for the RCE. "When TEFCA was initially designed, it primarily focused on basic treatment exchange. As we expand to payment, operations, individual access, and other purposes, we need governance structures that can accommodate these new exchange patterns without becoming unwieldy or creating unnecessary barriers."
As TEFCA expands beyond treatment exchange, its governance structures will need to evolve in several key ways. Governance frameworks may need to become more specific about requirements, processes, and oversight mechanisms for different exchange purposes. Governance bodies at all levels will need to incorporate perspectives from stakeholders focused on payment, operations, individual access, and other exchange purposes. Policies regarding data usage, consent, security, and other considerations may need to evolve to address the unique requirements of different exchange purposes. And monitoring, auditing, dispute resolution, and other operational governance functions will need to mature to handle increased complexity and volume.
Progress in governance evolution will likely follow an incremental path, with specific refinements being made to address emerging needs and challenges rather than wholesale restructuring. This incremental approach helps maintain stability while enabling adaptation to changing circumstances.
For TEFCA to successfully support comprehensive interoperability across multiple exchange purposes, its governance structures must strike a delicate balance: robust enough to ensure trust and reliability, flexible enough to accommodate diverse needs, and efficient enough to avoid creating excessive burdens that discourage participation.
## Stakeholder Perspectives: Diverse Needs and Motivations
Understanding TEFCA's potential to create comprehensive interoperability requires appreciating the diverse perspectives, needs, and motivations of different stakeholders in the healthcare ecosystem. These stakeholders approach TEFCA with varying priorities, concerns, and expectations that significantly influence their participation decisions and usage patterns.
Providers: Balancing Clinical Value and Operational Burden
Healthcare providers, including hospitals, physician practices, and health systems, represent primary participants in the TEFCA ecosystem. Their perspectives on TEFCA are shaped by several key considerations that influence their engagement with different exchange purposes.
Dr. James Wilson, Chief Medical Information Officer at a community hospital system, describes his organization's approach: "For us, TEFCA participation is primarily about improving patient care. We want to have a complete picture of our patients' health history, regardless of where they've received care before. But we're also conscious of the implementation costs and the potential impact on our clinical workflows. Any new exchange capabilities need to demonstrate clear clinical value without adding significant burden to our already-busy clinicians."
For providers, treatment exchange typically offers the clearest and most immediate value proposition. When a patient arrives in the emergency department or for a specialist consultation, access to their prior records can improve care quality, reduce duplicate testing, and enhance clinical decision-making. This direct clinical utility helps explain why provider participation in TEFCA has focused primarily on treatment exchange.
Other exchange purposes often present more complex value equations for providers, with benefits that may be less direct or accrue primarily to other stakeholders. Payment-related exchange might streamline administrative processes but could also increase scrutiny of clinical decisions. Operations exchange for quality improvement or population health could enhance organizational performance but requires investments in analytics capabilities to derive value from exchanged data. Individual access capabilities create potential benefits for patients but may generate additional support requirements for provider organizations.
"We're definitely interested in expanding beyond basic treatment exchange," notes Sarah Thompson, Chief Information Officer at a large physician group. "But each additional use case requires careful evaluation. What specific problem are we solving? What resources will it require from our team? How will it integrate with our existing workflows and systems? And ultimately, how will it benefit our patients and our organization? TEFCA needs to help us answer these questions clearly for each exchange purpose."
To expand provider engagement with broader exchange purposes, TEFCA implementation must address several key considerations: minimizing implementation burdens, ensuring clear value propositions, aligning with existing workflows, and creating appropriate incentives through payment models or regulatory requirements. Approaches that leverage existing capabilities while incrementally expanding functionality are likely to gain more traction than those requiring significant new investments or workflow changes.
Payers: Seeking Value Beyond Claims
Health insurers and other payers approach TEFCA with different priorities than providers, shaped by their focus on managing costs, assessing risk, ensuring appropriate utilization, and increasingly, supporting value-based care models.
"Claims data tells us what happened, but clinical data helps us understand why," explains Jennifer Chen, Vice President for Data Strategy at a regional health plan. "As we move toward more value-based arrangements, we need a comprehensive view of our members' health status and care patterns. That requires integrating clinical and financial data in ways that our traditional approaches don't fully support."
For payers, TEFCA offers potential value for several key objectives. Clinical data access could enhance risk adjustment accuracy, improve utilization management processes, and support more sophisticated care management programs. Standardized exchange could streamline administrative processes like prior authorization, claims adjudication, and provider credentialing. And as value-based arrangements grow, comprehensive data about members can support care coordination, quality measurement, and performance assessment across provider networks.
However, many payers have invested in their own data acquisition strategies, including direct connections with providers, private HIEs, or data aggregation services. These existing investments influence their assessment of TEFCA's value proposition. "We're watching TEFCA with interest," notes Robert Thompson, Chief Technology Officer at a national insurer. "But we already have significant investments in our own interoperability infrastructure. For us to shift toward TEFCA, it needs to offer clear advantages over our current approach—better data quality, more comprehensive coverage, or lower costs."
The relationship between payers and providers also influences TEFCA participation decisions. The historical tension between these stakeholders can create hesitation about sharing data through common infrastructure. "There's a fundamental trust issue that needs to be addressed," explains Dr. Michael Johnson, who works with both payers and providers on value-based care initiatives. "Providers worry that easier access to clinical data will just lead to more denials and audits. We need to demonstrate that better data exchange can actually reduce administrative burden and support more collaborative relationships focused on value and outcomes."
To increase payer engagement with TEFCA, implementation must address several key considerations: creating clear value propositions relative to alternative approaches, ensuring technical compatibility with payer systems, addressing trust concerns between payers and providers, and establishing appropriate governance frameworks for payment and operations exchange. Policy interventions, such as the CMS Interoperability and Prior Authorization Rule, can also help align incentives by establishing consistent requirements that make TEFCA participation more attractive.
Individuals: Seeking Agency in Their Health Journey
Individuals (patients and consumers) have distinct interests in health information exchange, centered on having access to their complete health information, controlling how it is shared, and using it to support their health and healthcare decisions.
"My health data is scattered across multiple systems," says Maria Rodriguez, who manages complex chronic conditions. "I have different patient portals for my primary care doctor, specialists, and hospital. Each has partial information, and none gives me the complete picture. When I switch doctors or seek care while traveling, I often have to start from scratch explaining my history. A truly national system that gives me access to all my health information would make a world of difference."
For individuals, TEFCA's individual access exchange purpose potentially offers significant value by creating a more comprehensive, standardized approach to accessing and sharing their health information. This could enhance their ability to manage their health, coordinate their own care across providers, detect errors in their records, and make more informed decisions. The ability to direct the sharing of their information with third-party applications or services could enable new tools and services that help them understand and use their health data more effectively.
However, realizing this potential requires addressing several challenges from the individual perspective. Many patients have limited awareness of their rights to access their health information or the potential benefits of health data access. Technical and administrative barriers, from complex identity verification processes to confusing interfaces, can discourage engagement. And concerns about privacy, security, and potential misuse of health information may create hesitation about broader sharing.
"The technical challenge is only part of the picture," notes Lisa Chen, a patient advocate. "We also need to address the usability challenge—making it easy for people with different levels of technical and health literacy to find, access, and use their health information. And we need to build trust through transparent privacy practices and meaningful individual control over how data is shared and used."
To better serve individual needs, TEFCA implementation must address several key considerations: creating user-friendly access mechanisms, ensuring appropriate identity verification that balances security with accessibility, developing clear consent models that provide meaningful control, and building trust through transparency and accountability. Educational resources to help individuals understand their rights, the value of health information access, and how to effectively use their data will also be important for driving adoption.
Public Health and Government Agencies: Pursuing Population Health Goals
Public health authorities and government agencies approach TEFCA with yet another distinct perspective, focused on population health monitoring, disease surveillance, program administration, and policy development.
"The COVID-19 pandemic highlighted both the critical importance of public health data exchange and the significant gaps in our current capabilities," observes Dr. Jennifer Lewis, an epidemiologist at a state health department. "We struggled to get comprehensive, timely data on cases, hospitalizations, and outcomes. We cobbled together multiple reporting systems, each with different formats, timing, and completeness. A robust national infrastructure that connects clinical data systems with public health could dramatically enhance our ability to monitor and respond to health threats."
For public health authorities, TEFCA offers potential value for enhancing disease surveillance, outbreak detection, population health monitoring, and program evaluation. Rather than relying on fragmented, often delayed reporting systems, public health agencies could have more complete, near-real-time visibility into health patterns and trends. This capability could improve responsiveness to emerging threats, enhance targeting of interventions, and support more effective resource allocation.
For government agencies involved in benefits determination, such as disability programs or veterans' benefits, TEFCA could streamline access to the clinical documentation needed to evaluate eligibility. This could reduce processing times for beneficiaries, decrease administrative costs for agencies, and potentially improve accuracy of determinations through more comprehensive information access.
However, these stakeholders face several challenges in engaging with TEFCA. Many public health authorities and government agencies operate with significant resource constraints that limit their ability to invest in new interoperability approaches without dedicated funding. Their existing data systems often use different technical standards and approaches than clinical systems, requiring additional integration work. And the governance frameworks needed to support public health and government exchange through TEFCA are still developing.
"There's also a significant workforce challenge," notes Dr. Lewis. "Many public health agencies have limited informatics expertise and are still working to modernize their basic data infrastructure. Participating in a sophisticated nationwide exchange network requires specialized skills that are in short supply in the public sector, particularly at state and local levels."
To increase public sector engagement with TEFCA, implementation must address several key considerations: aligning with existing public health data standards and systems, providing dedicated funding for implementation, developing governance processes that address public sector needs, and creating clear legal frameworks for appropriate data access. Federal leadership, including coordination across health-focused agencies like CDC, CMS, and ONC, will be essential for driving progress in this area.
Researchers: Advancing Knowledge Through Data Access
The research community represents another important stakeholder group with distinct perspectives on TEFCA's potential. Clinical researchers often struggle to access representative patient data across organizations, limiting their ability to address important research questions efficiently and comprehensively.
"Our current approach to research data access is incredibly inefficient," explains Dr. Robert Anderson, principal investigator for a multi-center clinical study. "For each study, we have to establish separate data sharing agreements with multiple organizations, navigate different IRB processes, and then deal with variations in how data is structured and defined. This slows down research, increases costs, and often limits the diversity and representativeness of our study populations. A nationwide infrastructure that standardizes these processes could dramatically accelerate biomedical research."
For researchers, TEFCA's research exchange purpose offers potential value by creating more standardized access to diverse clinical data sources. This could accelerate discoveries, enhance trial recruitment, improve representativeness of study populations, and enable more robust health services research. TEFCA could potentially serve as a foundation for a learning health system that systematically generates and applies evidence to improve care.
However, research exchange through TEFCA faces several implementation challenges. Research often requires more complex consent models than treatment exchange, particularly for secondary use of clinical data. Ensuring data quality, provenance, and semantic interoperability becomes even more critical when data will be used for research rather than direct patient care. And governance frameworks must carefully balance research access with privacy protection and address ethical considerations around data use.
"There's also the question of how research access through TEFCA would relate to other research data initiatives," notes Dr. Sarah Thompson, who leads informatics for a research network. "We already have the NIH's All of Us program, PCORnet, various disease-specific registries, and other research data networks. How would TEFCA complement or integrate with these existing structures rather than creating yet another parallel system?"
To support research through TEFCA effectively, implementation must address several key considerations: developing appropriate consent models for research use, ensuring data quality and provenance tracking, creating technical capabilities for cohort identification and longitudinal analysis, and establishing governance frameworks that balance research access with privacy protection. Coordination with existing research data initiatives will also be important to create an integrated ecosystem rather than isolated capabilities.
Headwinds and Tailwinds: Forces Shaping TEFCA's Evolution
As TEFCA continues to evolve, its trajectory will be shaped by various forces that either accelerate or impede progress toward comprehensive interoperability. Understanding these headwinds and tailwinds is essential for developing effective strategies to advance TEFCA's broader potential.
Technical Forces
Several technical factors create both challenges and opportunities for TEFCA's expansion beyond treatment exchange.
Technical Headwinds:
The persistence of legacy systems with limited interoperability capabilities creates significant barriers to participation for many healthcare organizations. "We're still running systems that were designed in an earlier era of healthcare IT," explains Michael Chen, IT Director at a rural health system. "Connecting these systems to modern exchange networks requires custom interfaces, data mapping, and often manual processes that strain our limited resources."
The ongoing transition from document-centric to API-based exchange creates implementation challenges as organizations must support multiple paradigms simultaneously. This transition requires new skills, tools, and approaches that many organizations are still developing.
Inconsistent data quality, terminology usage, and information models across systems complicate meaningful exchange and use of shared information. "Getting the bits and bytes to flow is only half the battle," notes Dr. Jennifer Smith, a clinical informaticist. "Making the exchanged data actually useful and meaningful in different contexts is much harder. Variations in how organizations document, code, and structure information create significant challenges for interoperability."
The lack of a national patient identifier continues to create challenges for reliable patient matching across disparate systems and organizations, particularly as exchange volumes grow and more diverse organizations participate.
Despite these challenges, several technical trends create momentum for expanded interoperability:
The continued maturation and adoption of the FHIR standard provides a stronger technical foundation for granular, API-based exchange across diverse use cases. "FHIR is transformative because it combines the technical advantages of modern web APIs with healthcare-specific data models," explains David Thompson, Chief Technology Officer at a health IT vendor. "This makes it much easier to create interoperable applications and services that can work across organizational boundaries."
Increasing adoption of cloud technologies in healthcare creates new opportunities for scalable, standardized exchange infrastructure. Cloud platforms can potentially reduce the implementation burden for smaller organizations while enabling more sophisticated exchange capabilities.
A growing ecosystem of healthcare applications creates demand for standardized data access across organizational boundaries, creating market pull for expanded interoperability. As these applications become more central to healthcare delivery and management, the pressure for comprehensive data access will likely increase.
Maturation of standards like SMART App Launch, UDAP, and OAuth 2.0 provides better foundations for secure, interoperable authentication and authorization. These capabilities are particularly important for expanding beyond treatment exchange to support individual access, third-party applications, and more diverse exchange participants.
Emerging capabilities in areas like artificial intelligence, natural language processing, and distributed computing create new opportunities to address long-standing challenges in areas like patient matching, data normalization, and consent management.
Operational Forces
Beyond technical considerations, several operational factors influence TEFCA's evolution toward comprehensive interoperability.
Operational Headwinds:
The multi-layered TEFCA framework creates significant implementation complexity that can be particularly challenging for smaller organizations with limited resources. "Just understanding the different agreements, policies, and technical requirements is a major undertaking," notes Sarah Williams, Compliance Officer at a community hospital. "For organizations without dedicated interoperability staff, this complexity can be overwhelming."
Integrating external information into existing clinical and administrative workflows remains difficult, limiting the practical utility of exchanged information. "If clinicians have to interrupt their normal workflow to access external data, or if the data isn't presented in a usable format within their existing systems, adoption will remain limited," explains Dr. Robert Johnson, a practicing physician and informatics leader.
The processes for onboarding new participants to QHINs, establishing connections, and validating capabilities can be time-consuming and resource-intensive. This creates barriers to participation, particularly for smaller organizations or those new to health information exchange.
Significant variations in operational maturity across healthcare organizations create challenges for establishing consistent, reliable exchange patterns. Organizations with limited experience in health information exchange often require significant support and guidance to implement even basic capabilities.
Operational Tailwinds:
Despite these challenges, several operational trends create momentum for expanded interoperability:
As organizations gain experience with basic exchange through TEFCA, they develop capabilities and processes that can support expansion to additional exchange purposes. This accumulated experience creates a foundation for incremental growth rather than requiring entirely new implementations for each exchange purpose.
Emerging best practices for TEFCA implementation and operation help reduce the "learning curve" for new participants. As the community develops implementation guides, case studies, and shared knowledge, the path to participation becomes clearer and more accessible.
Increasing automation of exchange processes, from patient matching to consent management to data transformation, reduces operational burdens and makes broader participation more feasible. These automation capabilities are particularly important for scaling beyond basic treatment exchange to support more complex exchange patterns.
Growing availability of implementation guides, tools, and support resources helps organizations navigate the complexities of TEFCA participation. These resources can be particularly valuable for smaller organizations or those with limited health IT expertise.
Ongoing workforce development in health IT and informatics creates a larger pool of professionals with the skills needed to implement and operate exchange capabilities. As these skills become more widely distributed across the healthcare ecosystem, the capacity for expanded interoperability grows.
Economic Forces
Economic factors create both significant challenges and opportunities for TEFCA's expansion beyond treatment exchange.
Economic Headwinds:
The misalignment of costs and benefits across stakeholders creates persistent challenges for interoperability investments. "In many cases, the organization bearing the cost of implementing and maintaining exchange capabilities isn't the one receiving the primary benefits," explains Dr. Michael Jefferson, a health economist. "This creates underinvestment relative to the societal value of comprehensive interoperability."
For many exchange purposes beyond treatment, the return on investment remains uncertain or difficult to quantify. This uncertainty makes it challenging for organizations to justify the required investments, particularly in resource-constrained environments.
Some organizations view health information as a competitive asset rather than a public good, creating resistance to broader sharing. "In many markets, control of patient data is seen as a way to keep patients within a particular health system or network," notes Jennifer Chen, a healthcare consultant. "More open exchange threatens that strategy, creating hesitation about participation in broader networks."
Developing sustainable, equitable fee structures for TEFCA participation that don't create barriers to entry presents ongoing challenges. Fee models that work for large health systems may be prohibitive for smaller providers, public health agencies, or consumer applications, limiting diversity of participation.
Public funding for interoperability infrastructure remains limited and often focused on specific programs rather than core infrastructure. This creates challenges for sustaining the basic capabilities needed for nationwide exchange, particularly as initial implementation funding diminishes.
Economic Tailwinds:
Despite these challenges, several economic trends create momentum for expanded interoperability:
The continued growth of value-based care models creates stronger financial incentives for comprehensive data sharing to support care coordination, quality improvement, and population health management. As organizations take on more financial risk for outcomes, the value of comprehensive data access increases.
Increasing pressure to reduce administrative costs in healthcare creates incentives to invest in more efficient, automated approaches to information exchange. Functions like prior authorization, claims adjudication, and quality reporting can potentially be streamlined through better interoperability, creating direct economic benefits.
Growing consumer expectations for digital access and convenience create market pressures for improved interoperability. Organizations that can offer seamless digital experiences, including comprehensive health information access, may gain competitive advantages in consumer-driven healthcare markets.
A growing ecosystem of healthcare innovation, from digital health startups to advanced analytics firms, creates demand for more comprehensive, standardized data access. As these innovative approaches demonstrate value, they create economic incentives for expanded interoperability.
Targeted public investments in interoperability infrastructure, while limited, provide essential seed funding for developing new capabilities and approaches. Strategic use of these investments can catalyze broader market adoption by reducing initial barriers and demonstrating value.
Policy Forces
Policy and regulatory factors create both challenges and opportunities for advancing TEFCA beyond treatment exchange.
Policy Headwinds:
The complex patchwork of federal and state privacy laws creates significant compliance challenges for nationwide exchange, particularly for sensitive information categories. "Navigating the variations between states, and between different types of health information, requires sophisticated legal and technical approaches that many organizations struggle to implement," explains Patricia Nguyen, a healthcare privacy attorney.
Uncertainty about how existing regulations apply to new exchange patterns or technologies can create hesitation among potential participants. Without clear guidance, many organizations take conservative approaches that limit data sharing even when it might be permitted.
Concerns about enforcement actions related to information blocking, privacy violations, or security breaches can create risk aversion among organizations considering expanded exchange. This regulatory risk may discourage innovation or participation in new exchange models.
Multiple, sometimes uncoordinated policy initiatives related to interoperability create implementation challenges for organizations trying to maintain compliance. "We're simultaneously trying to implement TEFCA, comply with information blocking rules, meet requirements for API access under the Interoperability and Patient Access Rule, and prepare for upcoming prior authorization requirements," notes Mark Johnson, Compliance Officer at a health system. "It's challenging to coordinate all these different initiatives with limited resources."
Shifting political priorities and leadership changes can create uncertainty about long-term policy direction and support for interoperability initiatives. This uncertainty makes it difficult for organizations to make strategic investments in capabilities that may depend on sustained policy commitment.
Policy Tailwinds:
Despite these challenges, several policy trends create momentum for expanded interoperability:
Increasing enforcement of information blocking provisions creates stronger incentives for organizations to facilitate appropriate information sharing. As enforcement actions and penalties become more concrete, organizations are more likely to prioritize interoperability capabilities.
Growing coordination among federal agencies around interoperability policy creates more coherent, aligned requirements and incentives. Initiatives like the Federal Health IT Coordinating Council help ensure that different agencies' requirements complement rather than conflict with each other.
Regulatory requirements for adopting specific interoperability standards create market momentum and reduce technical fragmentation. By establishing common technical foundations, these requirements make broader interoperability more feasible and less costly to implement.
Payment policies that reward care coordination, quality improvement, and population health management create indirect incentives for improved interoperability. As reimbursement increasingly depends on outcomes and efficiency, the financial case for comprehensive data access becomes stronger.
Growing regulatory emphasis on patient rights to access and control their health information creates pressure for improved individual access capabilities. These requirements align with consumer expectations and create demand for more comprehensive, user-friendly access mechanisms.
Pathways to Progress: Strategies for Advancing Comprehensive Interoperability
Building on this analysis of TEFCA's current state, stakeholder perspectives, and the forces shaping its evolution, several strategic pathways emerge for advancing TEFCA beyond treatment exchange toward more comprehensive interoperability.
Phased Expansion of Exchange Purposes
Rather than attempting to implement all exchange purposes simultaneously, a phased approach that systematically expands beyond treatment exchange offers several advantages.
"We need to be both ambitious in our vision and realistic in our implementation approach," explains Dr. Sarah Thompson, who advises healthcare organizations on interoperability strategy. "Each exchange purpose has its own technical, operational, and policy considerations. By tackling them in a thoughtful sequence, we can build on successes, learn from challenges, and maintain momentum toward the broader goal of comprehensive interoperability."
A phased approach allows exchange purposes to be prioritized based on technical readiness, policy clarity, stakeholder interest, and value potential. Experience gained from each expansion phase can inform subsequent phases, allowing for refinement of technical approaches, governance frameworks, and business models. Organizations can manage their implementation resources more effectively, avoiding overwhelming demands. And focused initiatives around specific exchange purposes can facilitate targeted stakeholder engagement and coalition-building.
One potential sequence for exchange purpose expansion might begin with continued strengthening of the treatment exchange foundation, then expand to support consumer-directed exchange (building on regulatory momentum around patient access rights), implement targeted healthcare operations use cases with clear value propositions (such as quality measurement or care coordination), address specific payment-related exchanges with high administrative burden (such as prior authorization or risk adjustment), develop focused public health and government benefits use cases aligned with agency priorities and funding opportunities, and establish frameworks for appropriate research access to TEFCA data with appropriate consent and governance.
This phased approach doesn't mean abandoning the comprehensive vision of TEFCA, but rather recognizes that different exchange purposes have different implementation requirements, stakeholder dynamics, and maturity timelines. By systematically expanding capabilities while maintaining a clear vision of the ultimate goal, TEFCA can make steady progress toward comprehensive interoperability.
Use Case Specificity
Complementing the phased approach, greater specificity around particular use cases within each exchange purpose can accelerate progress and demonstrate value.
"Abstract interoperability doesn't motivate action," notes Michael Torres, CEO of a health technology company. "Specific, concrete use cases that solve real problems for specific stakeholders—that's what drives adoption and investment. We need to identify the highest-value use cases within each exchange purpose and focus our initial efforts there."
Developing detailed technical, operational, and policy requirements for specific use cases provides clearer implementation guidance and reduces uncertainty. Well-defined use cases allow for clearer articulation of costs, benefits, and ROI for potential participants. Specific use cases create natural opportunities for bringing together the particular stakeholders needed for successful implementation. And defined use cases enable more precise measurement of progress and outcomes, supporting continuous improvement.
Examples of specific use cases that might be prioritized within each exchange purpose include:
For treatment: Transitions of care between hospitals and post-acute facilities, emergency department visits for patients with complex conditions, or specialist referrals with clinical decision support.
For individual access: Patient access to longitudinal health records across multiple providers, sharing records when changing providers or seeking second opinions, or directing data to personal health applications for monitoring chronic conditions.
For operations: Quality measure reporting for value-based payment programs, care gap identification for population health management, or provider directory maintenance to improve accuracy of referral networks.
For payment: Streamlining prior authorization for high-volume procedures, automating claims attachment submission, or enhancing risk adjustment data submission with clinical details.
For public health: Enhancing notifiable condition reporting with clinical details, supporting syndromic surveillance for emerging health threats, or improving immunization reporting completeness and timeliness.
For government benefits: Streamlining disability determination through structured clinical data access, improving program eligibility verification processes, or enhancing coordination between healthcare and social service programs.
For research: Supporting cohort identification for clinical trials, facilitating post-market surveillance studies of medical devices or medications, or enabling health services research on care patterns and outcomes.
By focusing on specific, high-value use cases within each exchange purpose, TEFCA implementation can build momentum through demonstrable successes that encourage broader participation. These targeted implementations can then expand over time to encompass additional use cases within each exchange purpose.
Technical Capability Evolution
Advancing TEFCA beyond treatment exchange requires evolution of its technical capabilities to support diverse exchange patterns and use cases.
"The initial TEFCA technical framework was built around document exchange because that's what existing networks were already doing," explains Miguel Rodriguez, Chief Technology Officer at a health information exchange. "But to support the full range of exchange purposes, we need to evolve toward more granular, API-based exchange that can support diverse applications and use cases."
Incorporating FHIR-based exchange alongside document exchange creates a more comprehensive technical foundation that supports both clinical and administrative use cases. Adding support for population-level data exchange enables more efficient operations, payment, public health, and research use cases. Enhanced directory capabilities for both technical endpoints and provider information facilitate more automated, reliable exchange connections. More sophisticated consent management capabilities enable exchange of sensitive information categories and support for more complex authorization models. And advanced identity matching and management solutions improve reliability and reduce the operational burden of patient matching across disparate systems.
This technical evolution should be pursued incrementally, with clear migration paths that maintain backward compatibility while enabling new capabilities. "We can't require everyone to jump to new standards all at once," notes Dr. Karen Chen, an interoperability specialist. "We need an approach that allows organizations to adopt newer capabilities at their own pace while ensuring that basic exchange continues to function."
Close coordination with standards development organizations, technology vendors, and implementers is essential to ensure that new capabilities are practical, interoperable, and aligned with broader industry trends. Technical evolution should also be guided by the specific requirements of prioritized use cases, ensuring that development efforts focus on capabilities that deliver tangible value.
Governance Evolution
As TEFCA expands beyond treatment exchange, its governance structures must evolve to address the unique considerations of diverse exchange purposes while maintaining a coherent overall framework.
"Governance is about creating the conditions for productive collaboration among diverse stakeholders," explains Dr. Robert Johnson, who serves on a QHIN governance committee. "As TEFCA encompasses more exchange purposes and stakeholders, governance becomes both more important and more challenging. We need structures that provide appropriate guardrails while enabling innovation and adaptation."
Developing more detailed policies for each exchange purpose can address unique requirements, stakeholder considerations, and risk profiles without requiring changes to the overall Common Agreement. Ensuring appropriate representation of stakeholders focused on different exchange purposes in governance bodies at all levels helps ensure that diverse perspectives are considered in decision-making. Establishing effective mechanisms for resolving disputes and addressing compliance issues across diverse exchange scenarios builds trust and accountability. Developing appropriate approaches to monitoring, measuring, and reporting on exchange activities across different purposes enables continuous improvement. And creating structured processes for gathering feedback, identifying issues, and implementing improvements based on implementation experience supports ongoing evolution.
This governance evolution should balance the need for consistent baseline requirements with appropriate flexibility to address the specific needs of different exchange purposes and stakeholders. It should also seek to minimize unnecessary administrative burdens while maintaining essential trust protections.
"Effective governance isn't about creating rigid rules," notes Elizabeth Chen, a governance specialist. "It's about establishing clear expectations, transparent processes, and appropriate accountability mechanisms that enable diverse organizations to work together effectively toward shared goals. As TEFCA expands to new exchange purposes, governance needs to evolve in ways that maintain trust while enabling innovation."
Economic Model Development
Advancing TEFCA beyond treatment exchange requires developing sustainable economic models that support diverse exchange purposes and ensure long-term viability.
"The economic challenge is fundamental to healthcare interoperability," explains Dr. Michael Jefferson, a health economist. "We need models that equitably distribute costs, align incentives, and create sustainable revenue streams for the infrastructure required. Without viable economic models, even the best technical and governance approaches will struggle to achieve widespread adoption."
Creating clearer articulations of the value propositions for different stakeholders and exchange purposes, quantifying benefits where possible, can help build the business case for participation. Exploring innovative fee structures that distribute costs equitably, reflect value received, and avoid creating barriers to participation can enhance sustainability. Developing strategies for targeted public investments in core infrastructure components that function as public goods can ensure essential capabilities while private markets develop sustainable models. Aligning TEFCA implementation with value-based payment models can create indirect incentives for appropriate data sharing. And supporting the development of diverse business models around TEFCA participation, including value-added services that enhance core exchange capabilities, can create multiple revenue streams to support the overall ecosystem.
This economic model development should recognize that different exchange purposes may require different financing approaches, reflecting their distinct value distribution patterns, stakeholder dynamics, and public interest considerations. Some exchange purposes with clear commercial value, such as certain payment-related exchanges, may be well-suited to market-based models. Others with broader public benefits but diffuse economic value, such as public health exchange, may require more significant public investment.
"We need to move beyond the false dichotomy of market versus government funding," argues Sarah Williams, Executive Director of a state-level HIE. "Core health information exchange infrastructure has characteristics of both private and public goods. Sustainable models will likely involve hybrid approaches that combine public investment in essential infrastructure with market-based models for value-added services."
Policy and Regulatory Levers
Strategic use of policy and regulatory levers can accelerate TEFCA's expansion beyond treatment exchange by addressing key barriers and aligning incentives across stakeholders.
"Policy interventions are essential catalysts for interoperability progress," notes Mark Johnson, a healthcare policy analyst. "While market forces and voluntary coordination play important roles, experience shows that significant advances in healthcare interoperability typically require policy action to overcome coordination problems, misaligned incentives, and market failures."
Targeted enforcement of information blocking provisions that emphasizes exchange purposes beyond treatment creates incentives for broader participation. Aligning federal and state health program requirements with TEFCA capabilities can create significant incentives for participation. Incorporating TEFCA-related capabilities into certification programs for health IT systems can accelerate technical adoption. Creating payment incentives or requirements related to interoperability can strengthen the business case for TEFCA participation. And efforts to harmonize privacy requirements across jurisdictions and information categories can reduce compliance complexity.
These policy interventions should be developed collaboratively with industry stakeholders to ensure they are practical, effective, and aligned with broader healthcare transformation goals. "Effective policy isn't developed in isolation," explains Patricia Nguyen, a healthcare attorney. "It requires deep understanding of market realities, technical capabilities, and operational considerations. The most effective interoperability policies build on industry progress while providing the necessary push to overcome persistent barriers."
Strategic coordination across federal agencies can enhance the impact of policy interventions. Alignment between ONC, CMS, CDC, FDA, and other health-focused agencies ensures that different policy initiatives reinforce rather than conflict with each other. Similarly, coordination between federal and state policies can reduce complexity and create more coherent incentives for comprehensive interoperability.
Conclusion: The Path Forward
TEFCA stands at a critical juncture in its evolution. It has established a functional foundation for nationwide health information exchange, primarily focused on treatment-related exchange between providers. Yet its broader promise—to create a comprehensive interoperability framework supporting diverse exchange purposes—remains largely unrealized.
The path forward requires recognizing both the complexity of the challenge and the imperative of the goal. Creating a truly nationwide health data utility that serves all stakeholders in the healthcare ecosystem involves navigating complex technical, operational, economic, and policy considerations. It requires balancing competing priorities, aligning diverse incentives, and managing legitimate tensions between information sharing and privacy protection.
Progress will likely be incremental rather than revolutionary, with specific use cases and exchange purposes advancing at different rates based on their unique dynamics. Treatment exchange will continue to mature and expand, while individual access, operations, payment, public health, government benefits, and research exchange will develop along their own trajectories, influenced by the specific headwinds and tailwinds they face.
Several principles can guide this evolution toward comprehensive interoperability:
First, purpose-driven design must remain central to implementation efforts. Focusing on specific use cases and stakeholder needs rather than abstract interoperability goals helps ensure that implementation efforts address real-world priorities and deliver tangible value. By starting with clear problems to solve and specific outcomes to achieve, TEFCA implementation can maintain momentum and demonstrate progress even as the broader vision evolves.
Second, balanced governance will be essential for managing an increasingly diverse ecosystem. Governance structures must balance the need for consistent baseline requirements with appropriate flexibility to address diverse stakeholder needs. As TEFCA encompasses more exchange purposes and participants, governance must become both more inclusive and more adaptable, incorporating new perspectives while maintaining the trust foundations essential for exchange.
Third, technical pragmatism should guide capability development. Technical approaches should build incrementally on existing capabilities while creating migration paths toward more advanced exchange patterns. This balanced approach allows organizations to adopt new capabilities at their own pace while ensuring continuity of basic exchange functions. It also recognizes the reality of limited implementation resources and the need to demonstrate value at each stage of evolution.
Fourth, economic realism must inform sustainability planning. Economic models must recognize the complex distribution of costs and benefits across the ecosystem and develop sustainable approaches to financing essential infrastructure. This may require creative combinations of public investment, participant fees, value-added services, and alignment with payment models to ensure long-term viability. Different exchange purposes may require different economic approaches reflecting their distinct value propositions and stakeholder dynamics.
Fifth, policy alignment can accelerate progress toward comprehensive interoperability. Policy interventions should create coherent, aligned incentives for appropriate information sharing while respecting legitimate privacy and security concerns. Strategic use of regulatory requirements, payment incentives, certification criteria, and enforcement actions can help overcome persistent barriers and create momentum for broader participation.
Successfully navigating this evolution requires continued collaboration among diverse stakeholders—providers, payers, technology vendors, policymakers, consumer advocates, and others—each bringing their unique perspectives and expertise to the challenge. It also requires sustained leadership from ONC, the RCE, and other key organizations to maintain momentum, address emerging challenges, and keep the focus on the broader vision of comprehensive interoperability.
Dr. Maria Rodriguez, a primary care physician who has seen decades of health IT evolution, offers a perspective that captures both the challenge and the opportunity: "Throughout my career, I've seen numerous attempts to solve healthcare's information sharing problems. Each has made some progress, but none has fully delivered on its promise. With TEFCA, we have perhaps our best opportunity yet to create a truly comprehensive approach. But success will require sustained commitment, willingness to address difficult issues, and keeping the focus on the ultimate goal—better care and better health for patients."
The ultimate measure of TEFCA's success will not be the volume of documents exchanged or the number of participants connected, but rather its impact on the fundamental goals of healthcare: better care, better health, lower costs, and improved experiences for patients and providers. By keeping these goals at the center of implementation efforts, TEFCA can evolve from its current state into a true nationwide health data utility that serves all stakeholders in the healthcare ecosystem.
The journey will not be easy or quick, but the potential rewards—a more connected, efficient, and effective healthcare system—make it worth pursuing with urgency, creativity, and determination. TEFCA's promise extends far beyond provider-to-provider treatment exchange, and realizing that broader promise remains one of the most important challenges and opportunities in health information technology today.
As we look to the future, we can envision a healthcare ecosystem where information flows seamlessly to support diverse needs: where clinicians have complete information about their patients regardless of where care was previously received; where patients can easily access and share their comprehensive health information through user-friendly interfaces; where administrative processes are streamlined through automated data exchange; where public health authorities have timely, comprehensive data to monitor and respond to health threats; where researchers can accelerate discoveries through efficient access to diverse data sources; and where government programs can serve beneficiaries more effectively through streamlined information access.
This vision remains aspirational, but TEFCA provides a foundation upon which it can be built. Through thoughtful evolution guided by clear principles and responsive to diverse stakeholder needs, TEFCA can gradually expand beyond its current focus to fulfill its broader promise of comprehensive nationwide interoperability. The path will require patience, persistence, and pragmatism—but the destination remains worthy of the journey.