The Empowered Patient: Reimagining Primary Care Through Validated Self-Research and AI-Assisted Medicine
Disclaimer: The views and opinions expressed in this essay are solely my own and do not reflect the official policy or position of my employer or any organization with which I am affiliated.
Abstract
The traditional primary care model faces unprecedented challenges: physician burnout, patient dissatisfaction, rising costs, and limited appointment time. Meanwhile, patients increasingly turn to internet searches and AI tools for health information, often without clinical validation. This essay proposes a revolutionary business model that bridges this gap by empowering patients to conduct structured, AI-assisted research under physician supervision, followed by clinical validation and comprehensive treatment pathways. This model transforms the doctor-patient relationship from a traditional paternalistic approach to a collaborative partnership, potentially improving outcomes while creating new revenue streams and operational efficiencies. The proposed framework includes community-driven research platforms, AI-powered symptom analysis tools, and integrated clinical validation systems that maintain safety while respecting patient autonomy and intelligence.
Table of Contents
1. Introduction: The Crisis in Primary Care
2. The Rise of Patient Self-Research
3. The Untapped Potential of AI in Patient Education
4. A New Business Model: The Collaborative Care Framework
5. Clinical Validation: The Safety Net
6. Technology Infrastructure and Implementation
7. Economic Implications and Revenue Models
8. Addressing Concerns and Limitations
9. Case Studies and Early Adopters
10. The Future of Empowered Healthcare
11. Conclusion: Toward a More Informed Partnership
---
Introduction: The Crisis in Primary Care
Primary care medicine stands at a crossroads. Physicians report unprecedented levels of burnout, with many leaving the profession entirely or reducing their patient loads. Patients express frustration with rushed appointments, limited access to specialists, and the feeling that their concerns are not adequately addressed. The average primary care appointment lasts just fifteen minutes, barely enough time to address a single complex health concern, let alone provide comprehensive education about conditions and treatment options.
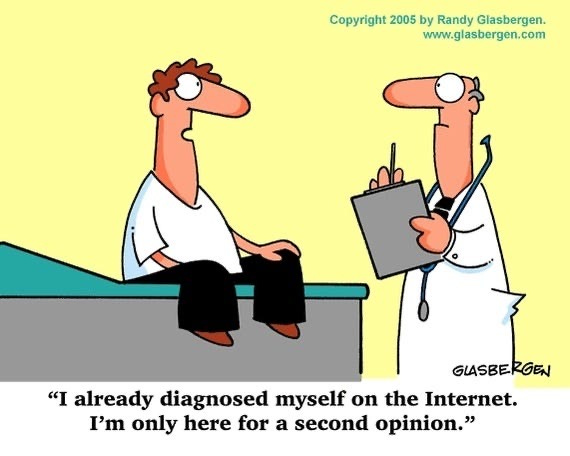
This time constraint has created a problematic dynamic where patients leave appointments with more questions than answers, often turning to unreliable internet sources for information. Dr. Google has become the world's most consulted physician, yet the information patients find online is rarely filtered through clinical expertise or personalized to their specific circumstances. This creates a dangerous gap between patient curiosity and clinical validation, leading to anxiety, misinformation, and potentially harmful self-treatment.
The traditional fee-for-service model exacerbates these problems by incentivizing volume over quality, pushing physicians to see more patients in less time rather than investing in meaningful patient education and engagement. Meanwhile, patients increasingly expect to be active participants in their healthcare decisions, armed with information and seeking collaborative relationships with their providers rather than passive compliance with medical directives.
The healthcare technology sector has responded with various solutions, from telemedicine platforms to symptom checker apps, but most of these tools operate in isolation from clinical care. Patients use them independently, without physician oversight, creating parallel healthcare experiences that may conflict with or undermine professional medical advice. What's missing is a business model that harnesses patient motivation for self-research while maintaining the safety and expertise of clinical oversight.
The opportunity before us is to create a new paradigm that transforms patient research from a liability into an asset, channeling natural curiosity and the power of AI into a structured, clinically validated process that enhances rather than threatens the physician-patient relationship. This approach recognizes that informed patients are better patients, and that the combination of human intelligence, artificial intelligence, and clinical expertise can create outcomes superior to any single component alone.
The Rise of Patient Self-Research
The digital revolution has fundamentally altered patient behavior and expectations. Studies consistently show that over ninety percent of patients research their symptoms online before or after seeing a physician. This behavior spans all age groups, education levels, and socioeconomic backgrounds, representing a fundamental shift in how people approach their health concerns.
Modern patients arrive at appointments with printouts from medical websites, questions generated by AI chatbots, and hypotheses about their conditions based on symptom matching algorithms. Rather than viewing this as a threat to physician authority, progressive healthcare providers are beginning to recognize it as an opportunity to engage patients more meaningfully in their own care.
The quality of patient self-research has improved dramatically with advances in AI and natural language processing. Tools like large language models can now provide sophisticated medical information, explain complex conditions in accessible language, and even suggest questions patients should ask their physicians. However, these tools operate without clinical context, personal medical history, or the nuanced understanding that comes from years of medical training and experience.
Patient communities have also emerged as powerful sources of information and support. Online forums dedicated to specific conditions often contain detailed discussions of symptoms, treatments, and outcomes that may not be found in medical literature. Patients share their experiences with different medications, describe side effects, and provide practical advice for managing chronic conditions. This collective knowledge represents a valuable resource that is typically disconnected from clinical care.
The challenge lies not in discouraging patient research but in channeling it productively. Patients who feel empowered to research their conditions and participate actively in treatment decisions show better adherence to medical recommendations and improved health outcomes. They ask more informed questions, better understand the rationale behind treatment decisions, and are more likely to follow through with recommended lifestyle changes.
However, unsupervised patient research can also lead to problems. Medical anxiety increases when patients encounter rare or serious conditions that match their symptoms. They may focus on alarming possibilities while ignoring more likely explanations. Without clinical training, patients may misinterpret medical information or draw incorrect conclusions from incomplete data.
The key insight is that patient research behavior is not going to disappear, regardless of physician preferences. The question is whether healthcare providers will find ways to harness this energy constructively or continue to treat it as a complication to be managed. The most successful approach will likely involve structured frameworks that guide patient research while maintaining clinical oversight and validation.
The Untapped Potential of AI in Patient Education
Artificial intelligence has reached a level of sophistication that makes it genuinely useful for patient education and preliminary health assessment. Modern AI systems can process vast amounts of medical literature, identify patterns in symptoms, and provide personalized health information that was previously accessible only to trained medical professionals.
The capabilities of AI in healthcare education extend far beyond simple symptom checking. Advanced language models can explain complex medical concepts in language appropriate to a patient's education level, cultural background, and personal circumstances. They can generate questions that patients should ask their physicians, help patients understand potential treatment options, and even assist in tracking symptoms over time.
AI excels at pattern recognition and data synthesis, capabilities that complement human clinical judgment rather than replacing it. While a physician might remember similar cases from their personal experience, AI can analyze patterns across millions of patient records, identifying correlations and insights that might not be apparent to individual practitioners. This creates opportunities for AI to serve as a research assistant for both patients and physicians.
The personalization capabilities of AI are particularly valuable in patient education. Rather than providing generic information about a condition, AI can tailor explanations based on a patient's specific symptoms, medical history, and personal circumstances. It can identify which aspects of a condition are most relevant to a particular patient and focus educational efforts accordingly.
AI can also serve as a bridge between patient communities and clinical care. By analyzing discussions in patient forums and support groups, AI systems can identify common concerns, effective coping strategies, and potential safety issues that should be brought to clinical attention. This creates a feedback loop where community knowledge informs clinical practice and clinical insights enhance community discussions.
The temporal advantages of AI are significant for patient education. Unlike physicians, who are available only during scheduled appointments, AI systems can provide immediate responses to patient questions and concerns. This immediacy can reduce anxiety and help patients make more informed decisions about when to seek medical attention.
However, the power of AI in patient education is only realized when it operates within appropriate clinical frameworks. AI systems lack the nuanced understanding of individual patient circumstances that comes from clinical experience. They cannot perform physical examinations, interpret subtle symptoms, or make the complex judgments that define medical practice. The value of AI lies in its ability to enhance and support clinical decision-making rather than replace it.
The most promising applications of AI in patient education involve structured collaboration between AI systems, patients, and physicians. AI can help patients prepare for appointments by generating relevant questions, organizing symptom information, and providing background education about their conditions. Physicians can then focus their limited appointment time on clinical assessment, interpretation of AI-generated insights, and collaborative decision-making about treatment options.
A New Business Model: The Collaborative Care Framework
The Collaborative Care Framework represents a fundamental reimagining of primary care delivery, built around the principle that informed patients are better patients. Rather than viewing patient research as a threat to clinical authority, this model embraces it as a valuable component of the diagnostic and treatment process.
At its core, the framework consists of three integrated components: structured patient research, clinical validation, and collaborative treatment planning. Each component builds upon the others to create a comprehensive care experience that leverages both human and artificial intelligence while maintaining clinical safety and effectiveness.
The structured patient research component provides patients with access to AI-powered tools designed specifically for health-related research. These tools go beyond simple symptom checkers to include comprehensive condition databases, treatment option explorers, and personalized health education modules. Patients can research their symptoms, explore potential diagnoses, and learn about treatment options in a structured environment designed to promote accurate understanding rather than anxiety.
The research tools are designed with clinical validation in mind. Rather than providing definitive diagnoses or treatment recommendations, they help patients organize their symptoms, identify relevant questions, and prepare for productive clinical conversations. The AI systems guide patients through systematic symptom documentation, help them understand the significance of different symptoms, and identify when immediate medical attention may be warranted.
Community features allow patients to connect with others who have similar conditions or symptoms, creating support networks that extend beyond individual clinical relationships. These communities are moderated by healthcare professionals and AI systems to ensure accuracy and safety while preserving the peer support that many patients find valuable.
The clinical validation component ensures that all patient research is reviewed and interpreted by qualified healthcare professionals. Physicians receive structured summaries of patient research activities, including symptom documentation, condition exploration, and community interactions. This information is integrated with traditional clinical data to provide a more comprehensive picture of each patient's health status and concerns.
The validation process is designed to be efficient and scalable. Rather than requiring physicians to review raw research data, AI systems pre-process patient research to identify key insights, potential concerns, and areas requiring clinical attention. This allows physicians to focus on interpretation and decision-making rather than data collection and organization.
Collaborative treatment planning involves patients and physicians working together to develop treatment strategies that incorporate both clinical expertise and patient preferences. Patients arrive at appointments with a deeper understanding of their conditions and treatment options, enabling more sophisticated discussions about care plans. Physicians can focus on clinical assessment and shared decision-making rather than basic education about conditions and treatments.
The economic model of the Collaborative Care Framework differs significantly from traditional fee-for-service approaches. Rather than billing primarily for face-to-face encounters, the framework creates multiple revenue streams including technology platform subscriptions, extended care coordination services, and outcome-based payment arrangements.
Patient engagement in the framework is voluntary but incentivized through improved access to information, enhanced physician relationships, and better health outcomes. Patients who participate in structured research activities receive more comprehensive care coordination, extended access to clinical support, and personalized health education resources.
The framework is designed to be scalable across different practice settings and patient populations. Small primary care practices can implement basic versions of the framework using cloud-based AI tools and community platforms. Large healthcare systems can develop more sophisticated implementations with integrated electronic health records and specialized care coordination teams.
Technology infrastructure supports the framework through secure, HIPAA-compliant platforms that integrate patient research activities with clinical workflows. AI systems provide real-time analysis of patient research, identify potential safety concerns, and generate insights that enhance clinical decision-making.
Clinical Validation: The Safety Net
The clinical validation component of the Collaborative Care Framework serves as the essential safety net that distinguishes this model from unstructured patient self-research. This systematic approach ensures that all patient-generated research and insights are filtered through clinical expertise before informing treatment decisions.
Clinical validation operates on multiple levels, from automated safety screening to comprehensive physician review. AI systems continuously monitor patient research activities for potential red flags, including symptoms that may indicate serious conditions, medication interactions, or concerning patterns of behavior. When these systems identify potential safety issues, they immediately alert clinical staff and may restrict certain research activities until professional review is completed.
The validation process begins with structured data collection. As patients research their symptoms and conditions, the AI systems organize this information into standardized clinical formats that physicians can quickly review and interpret. This includes symptom timelines, severity assessments, functional impact measures, and patient concerns organized by clinical priority.
Physicians receive comprehensive but concise summaries of patient research activities prior to scheduled appointments. These summaries highlight key findings, potential diagnoses suggested by AI systems, treatment options explored by patients, and specific questions or concerns that require clinical attention. This allows physicians to prepare for appointments more effectively and focus their limited time on the most clinically relevant issues.
The validation process also includes systematic review of patient-generated hypotheses about their conditions. While patients may develop theories about their symptoms based on online research, these hypotheses are evaluated against clinical standards and the physician's assessment of the patient's condition. This creates opportunities for valuable educational discussions about diagnostic reasoning and the limitations of self-diagnosis.
Community interactions require special validation protocols to ensure safety while preserving the peer support benefits of patient communities. AI systems monitor community discussions for medical misinformation, potentially harmful advice, and signs of medical emergencies. Healthcare professionals moderate these communities to provide accurate information and redirect serious medical concerns to appropriate clinical channels.
The validation framework includes specific protocols for different types of patient research. Symptom tracking and documentation are validated for accuracy and completeness. Medication research is reviewed for potential interactions and contraindications. Treatment option exploration is evaluated for safety and appropriateness. Lifestyle modification research is assessed for potential benefits and risks.
Quality assurance measures ensure that the validation process itself maintains high standards. Regular audits of AI system performance identify areas where automated screening may miss important safety concerns. Physician feedback on the usefulness and accuracy of research summaries helps refine the validation algorithms. Patient outcome data provides evidence about the effectiveness of the collaborative care approach.
The validation process is designed to be educational for both patients and physicians. When patient research identifies potential concerns that prove to be unfounded, the validation process becomes an opportunity to explain why certain symptoms are not worrisome and how to distinguish between serious and benign conditions. When patient research identifies legitimate concerns that might have been missed, it reinforces the value of the collaborative approach.
Emergency protocols ensure that the validation process does not delay necessary medical care. AI systems are programmed to identify symptoms that may indicate medical emergencies and immediately direct patients to appropriate care while simultaneously alerting their primary care physicians. These protocols are regularly updated based on clinical guidelines and outcome data.
The validation framework also addresses the challenge of health anxiety that can be exacerbated by medical research. When patients develop excessive worry about their symptoms based on online research, the validation process includes specific interventions to address these concerns and provide reassurance when appropriate.
Technology Infrastructure and Implementation
The technology infrastructure supporting the Collaborative Care Framework requires sophisticated integration of multiple systems while maintaining simplicity and accessibility for both patients and physicians. The platform architecture must support real-time AI analysis, secure data management, seamless clinical workflow integration, and scalable community features.
The core platform is built on cloud-based infrastructure that ensures reliability, security, and scalability. Patient research activities are supported by advanced natural language processing systems that can understand medical terminology, interpret symptom descriptions, and provide relevant educational content. These AI systems are trained on comprehensive medical databases and continuously updated with new research and clinical guidelines.
The patient interface is designed to be intuitive and accessible across different devices and technical skill levels. Patients can access the platform through web browsers, mobile applications, or tablet interfaces, with features optimized for each platform. The interface guides patients through structured research activities while providing flexibility for individual exploration and learning.
Symptom tracking capabilities allow patients to document their symptoms systematically over time, including severity ratings, timing patterns, and functional impacts. The AI systems analyze this data to identify trends and patterns that may not be apparent to patients or physicians during brief appointments. This longitudinal data provides valuable insights into condition progression and treatment effectiveness.
The educational content delivery system provides personalized health information based on patient symptoms, medical history, and research activities. AI systems curate relevant articles, videos, and interactive content from reputable medical sources, adapting the complexity and focus of the material to individual patient needs and preferences.
Community platform features enable patients to connect with others who have similar conditions while maintaining privacy and security. These communities include discussion forums, peer support groups, and educational webinars moderated by healthcare professionals. AI systems monitor community interactions to identify valuable insights and potential safety concerns.
Clinical workflow integration ensures that patient research activities enhance rather than complicate physician workflows. The platform generates structured reports that integrate with electronic health record systems, providing physicians with comprehensive but concise summaries of patient research activities. These reports are designed to save time during appointments while improving the quality of clinical discussions.
The AI analysis engine processes patient research activities in real-time, identifying patterns, potential concerns, and areas requiring clinical attention. Machine learning algorithms continuously improve the accuracy of these analyses based on clinical outcomes and physician feedback. The system learns from each patient interaction to provide better insights and recommendations over time.
Data security and privacy protections are built into every aspect of the platform architecture. All patient data is encrypted both in transit and at rest, with access controls that ensure only authorized healthcare providers can view sensitive information. The platform complies with HIPAA requirements and other relevant privacy regulations while enabling the collaborative features that make the framework effective.
Integration with existing healthcare systems is facilitated through standard APIs and data exchange protocols. The platform can connect with electronic health records, laboratory systems, pharmacy networks, and other healthcare technology platforms to provide a comprehensive view of patient health status and care coordination.
Mobile health features extend the platform capabilities to smartphone and wearable devices, enabling passive collection of health data such as activity levels, sleep patterns, and vital signs. This data is integrated with patient research activities to provide a more complete picture of health status and condition progression.
The platform includes robust analytics capabilities that provide insights into patient engagement, research patterns, and clinical outcomes. These analytics help healthcare providers optimize their use of the framework and identify opportunities for improvement in patient care and system performance.
Quality assurance systems continuously monitor platform performance, identify technical issues, and ensure that AI systems are providing accurate and helpful information. Regular updates and improvements are deployed based on user feedback, clinical outcomes, and advances in medical knowledge and technology.
Economic Implications and Revenue Models
The Collaborative Care Framework creates multiple new revenue streams while potentially reducing costs through improved efficiency and patient outcomes. The economic model shifts from traditional fee-for-service billing toward value-based care arrangements that reward patient engagement and health outcomes.
The primary revenue model involves subscription-based access to the technology platform and clinical validation services. Patients pay monthly or annual fees for access to AI-powered research tools, community features, and enhanced clinical support. These subscriptions provide predictable revenue streams that allow healthcare providers to invest in technology infrastructure and care coordination services.
Healthcare providers can offer different tiers of service based on patient needs and preferences. Basic subscriptions might include access to educational content and symptom tracking tools, while premium subscriptions could include personalized AI analysis, community access, and extended clinical support. This tiered approach allows providers to serve different patient populations while maximizing revenue potential.
The framework also creates opportunities for outcome-based payment arrangements with insurance companies and healthcare systems. Providers who demonstrate improved patient outcomes, reduced emergency department visits, or better management of chronic conditions can negotiate performance bonuses or shared savings arrangements.
Care coordination services represent another significant revenue opportunity. The framework enables providers to offer extended support services such as medication management, lifestyle coaching, and care navigation that complement traditional clinical encounters. These services can be billed separately or included in comprehensive care packages.
The technology platform itself can generate revenue through licensing arrangements with other healthcare providers or health systems. Successful implementations of the framework can be scaled and replicated across different practice settings, creating opportunities for technology licensing and consulting services.
Corporate wellness programs represent a growing market for the Collaborative Care Framework. Employers increasingly recognize the value of engaged, informed employees who take active roles in managing their health. The framework can be adapted for workplace wellness initiatives, creating new revenue streams while improving employee health outcomes.
The economic benefits of the framework extend beyond direct revenue generation. Improved patient engagement and education can lead to better treatment adherence, reduced complications, and fewer emergency interventions. These improvements translate into cost savings that can be shared between patients, providers, and insurance companies.
The framework also creates efficiencies in clinical workflows that can reduce operational costs. When patients arrive at appointments with structured symptom documentation and relevant research, physicians can focus on clinical assessment and decision-making rather than basic information gathering. This efficiency allows providers to see more patients or spend more quality time with each patient.
Reduced liability exposure represents another potential economic benefit. When patients are actively engaged in their care and fully informed about their conditions and treatment options, they are less likely to pursue malpractice claims. The documentation provided by the framework also creates clear records of patient education and informed consent processes.
The framework enables providers to capture and monetize the value of patient research activities that currently occur outside of clinical settings. Rather than viewing patient research as a complication to be managed, the framework transforms it into a billable service that enhances care quality and patient satisfaction.
Partnership opportunities with pharmaceutical companies and medical device manufacturers can create additional revenue streams. The framework generates valuable data about patient experiences with different treatments, medication adherence patterns, and outcome measures that can inform product development and marketing strategies.
The economic sustainability of the framework depends on demonstrating clear value to all stakeholders. Patients must perceive sufficient benefit from the enhanced services to justify subscription costs. Physicians must experience improved efficiency and patient outcomes that justify the investment in technology and training. Insurance companies must see reduced costs or improved outcomes that justify coverage of framework services.
Addressing Concerns and Limitations
The Collaborative Care Framework faces several legitimate concerns and limitations that must be addressed for successful implementation. These challenges range from regulatory compliance and liability issues to concerns about health equity and the potential for increased health anxiety.
Medical liability represents a primary concern for physicians considering the framework. When patients conduct extensive research about their conditions and participate actively in treatment decisions, questions arise about responsibility for outcomes and the potential for malpractice claims. The framework addresses these concerns through comprehensive documentation of patient education, informed consent processes, and clinical validation of all patient research activities.
The liability framework includes clear protocols for different types of patient research and clinical validation. Physicians retain ultimate responsibility for diagnosis and treatment decisions, while the framework provides structured support for patient education and engagement. Documentation systems ensure that all patient interactions are recorded and that appropriate clinical standards are maintained.
Regulatory compliance presents ongoing challenges as healthcare regulations evolve to address new technologies and care delivery models. The framework must comply with HIPAA privacy requirements, FDA regulations for medical devices and AI systems, and state medical practice requirements. Ongoing legal and regulatory consultation ensures that the framework remains compliant as regulations change.
Health equity concerns arise from the potential for the framework to exacerbate existing disparities in healthcare access and quality. Patients with limited digital literacy, language barriers, or socioeconomic constraints may be unable to participate fully in the framework. Implementation strategies must address these concerns through multilingual support, digital literacy training, and alternative access methods.
The framework includes specific provisions for addressing health equity concerns. Community health centers and safety net providers receive subsidized access to the technology platform. Multilingual AI systems provide support for non-English speaking patients. Digital literacy training programs help patients develop the skills needed to participate effectively in the framework.
Health anxiety represents a significant concern when patients have increased access to medical information. Some patients may become excessively worried about their symptoms or develop hypochondriacal behaviors when exposed to detailed medical information. The framework addresses these concerns through structured educational approaches, anxiety screening protocols, and referral pathways for patients who develop problematic health anxiety.
The AI systems include specific algorithms designed to identify and address health anxiety. When patients demonstrate excessive worry or obsessive research behaviors, the system provides appropriate interventions and may recommend professional mental health support. Clinical validation processes include specific protocols for addressing anxiety-related concerns.
Quality control of AI systems presents ongoing challenges as these technologies continue to evolve. Medical knowledge changes constantly, and AI systems must be regularly updated to reflect current clinical guidelines and research findings. The framework includes robust quality assurance processes to ensure that AI systems provide accurate and up-to-date information.
Physician resistance to the framework may arise from concerns about time requirements, technology complexity, or changes to traditional practice patterns. Implementation strategies must address these concerns through comprehensive training programs, workflow optimization, and demonstration of clinical and economic benefits.
The framework includes extensive physician support systems, including training programs, technical support, and peer mentorship opportunities. Physicians who successfully implement the framework serve as champions and mentors for other providers considering adoption.
Data security and privacy concerns require ongoing attention as the framework handles sensitive health information across multiple platforms and systems. Cybersecurity threats continue to evolve, and the framework must maintain robust security measures while enabling the collaborative features that make it effective.
Integration challenges arise when implementing the framework across different healthcare systems with varying electronic health records, workflow patterns, and technology capabilities. The platform must be sufficiently flexible to accommodate different implementation environments while maintaining core functionality and safety features.
The framework addresses integration challenges through modular design approaches that allow customization for different healthcare environments. Standard APIs enable integration with existing systems, while implementation support services help healthcare providers adapt the framework to their specific needs.
Case Studies and Early Adopters
Several pioneering healthcare organizations have begun implementing elements of the Collaborative Care Framework, providing valuable insights into the practical challenges and benefits of this approach. These early adopters demonstrate the potential for the framework while highlighting areas that require further development and refinement.
A community health center in rural Oregon implemented a basic version of the framework to address the challenges of serving a geographically dispersed patient population with limited specialist access. Patients use AI-powered symptom tracking and research tools between appointments, with clinical validation provided through secure messaging and periodic telehealth consultations.
The Oregon implementation focused on chronic disease management, particularly diabetes and hypertension. Patients track their symptoms, blood pressure readings, and medication adherence using the platform, while AI systems identify patterns and potential concerns that require clinical attention. The clinical validation process involves nurses and physicians reviewing AI-generated reports and providing feedback to patients through secure messaging.
Results from the Oregon implementation show improved patient engagement, better medication adherence, and reduced emergency department visits. Patients report feeling more informed about their conditions and more confident in managing their health. Physicians report that the structured patient research saves time during appointments and enables more focused clinical discussions.
A large urban primary care practice in Chicago implemented a more comprehensive version of the framework, including community features and extended clinical validation services. The practice serves a diverse patient population with varying levels of digital literacy and health knowledge, providing insights into the challenges of implementing the framework across different patient populations.
The Chicago implementation includes multilingual AI systems and digital literacy training programs to address health equity concerns. Community health workers provide support for patients who need assistance using the technology platform, while bilingual clinical staff ensure that all patients receive appropriate clinical validation of their research activities.
The practice reports significant improvements in patient satisfaction and clinical outcomes. Patients with chronic conditions show better self-management behaviors and reduced complications. The framework has enabled the practice to provide more comprehensive care coordination services while maintaining efficiency in clinical workflows.
A large health system in Boston piloted the framework across multiple primary care practices, providing insights into the challenges of implementing the framework at scale. The pilot included extensive training programs for physicians and staff, integration with existing electronic health record systems, and comprehensive outcome measurement.
The Boston pilot demonstrated the importance of physician buy-in and proper training for successful implementation. Practices that invested in comprehensive training and workflow optimization showed better results than those that implemented the framework without adequate preparation. The pilot also highlighted the need for ongoing technical support and quality assurance measures.
A specialty clinic focused on rheumatology in Seattle implemented the framework to address the challenges of managing complex chronic conditions that require extensive patient education and ongoing monitoring. The clinic serves patients with conditions such as rheumatoid arthritis and lupus, which require sophisticated understanding of symptoms, treatments, and lifestyle modifications.
The Seattle implementation demonstrates the potential for the framework to enhance specialist care by enabling more informed patient discussions and better self-management of chronic conditions. Patients report feeling more empowered to manage their conditions and more confident in their treatment decisions. The clinic has been able to extend time between appointments for stable patients while maintaining close monitoring through the platform.
A direct primary care practice in Austin, Texas, implemented the framework as part of a membership-based care model. Patients pay monthly membership fees that include access to the technology platform, unlimited clinical consultations, and comprehensive care coordination services. This model demonstrates the potential for subscription-based revenue models to support the framework.
The Austin implementation shows how the framework can enable innovative care delivery models that prioritize patient engagement and relationship building. The practice reports higher patient satisfaction scores and better clinical outcomes compared to traditional fee-for-service models. The subscription model provides predictable revenue that allows the practice to invest in technology and care coordination services.
These early implementations provide valuable lessons for broader adoption of the framework. Successful implementations require comprehensive training programs, ongoing technical support, and strong physician leadership. The framework works best when it is integrated into existing clinical workflows rather than implemented as an add-on service.
The case studies also demonstrate the importance of addressing health equity concerns through targeted support for underserved populations. Digital literacy training, multilingual support, and community health worker involvement are essential for ensuring that the framework benefits all patients rather than exacerbating existing disparities.
The Future of Empowered Healthcare
The Collaborative Care Framework represents just the beginning of a fundamental transformation in how healthcare is delivered and experienced. As artificial intelligence capabilities continue to advance and patient expectations evolve, the framework will likely expand to encompass even more sophisticated forms of patient empowerment and clinical collaboration.
Future developments in AI technology will enable more personalized and precise patient education and support. Machine learning algorithms will become better at understanding individual patient needs, learning preferences, and health behaviors. This will enable AI systems to provide increasingly tailored recommendations and support that adapt to each patient's unique circumstances and goals.
The integration of genomic information into the framework will enable truly personalized medicine approaches where patient research and education are tailored to individual genetic profiles. Patients will be able to understand how their genetic makeup influences their health risks and treatment responses, enabling more informed decisions about prevention and treatment strategies.
Wearable technology and continuous monitoring devices will provide real-time health data that can be integrated into the framework to provide more comprehensive and timely insights. Patients will be able to track their health status continuously, with AI systems identifying patterns and potential concerns that require clinical attention.
The framework will likely expand beyond primary care to encompass specialty care, mental health services, and preventive care. Specialists will be able to leverage patient research and education to provide more efficient and effective care, while patients will arrive at specialty appointments with sophisticated understanding of their conditions and treatment options.
Population health applications of the framework will enable healthcare systems to identify trends and patterns across large patient populations. This information can inform public health initiatives, clinical guideline development, and resource allocation decisions. The framework will become a valuable source of real-world evidence about treatment effectiveness and patient outcomes.
The global application of the framework has the potential to address healthcare access challenges in underserved regions. AI-powered patient education and clinical validation can extend the reach of limited healthcare resources, enabling patients in remote areas to receive sophisticated health information and support.
Integration with social determinants of health will enable the framework to address the broader factors that influence patient health outcomes. AI systems will be able to identify social, economic, and environmental factors that impact patient health and provide targeted interventions and support.
The framework will likely evolve to include predictive analytics that can identify patients at risk for developing certain conditions or experiencing health complications. This predictive capability will enable proactive interventions and prevention strategies that can improve outcomes while reducing costs.
Professional education and training will need to evolve to prepare healthcare providers for this new model of collaborative care. Medical schools and residency programs will need to teach skills in patient education, shared decision-making, and technology integration. Continuing education programs will help practicing physicians adapt to the changing healthcare environment.
Regulatory frameworks will need to evolve to address the new challenges and opportunities created by AI-powered healthcare and patient empowerment. This will require collaboration between healthcare providers, technology companies, and regulatory agencies to ensure that innovations are safe and effective while not stifling beneficial developments.
The economic models supporting healthcare will continue to evolve toward value-based care arrangements that reward patient engagement and outcomes rather than volume of services. The framework will play a crucial role in demonstrating the value of patient empowerment and collaborative care approaches.
Research and development in the healthcare technology sector will increasingly focus on tools and platforms that enhance rather than replace human healthcare providers. The most successful innovations will be those that strengthen the patient-provider relationship while improving efficiency and outcomes.
The ultimate vision for the framework is a healthcare system where patients are truly empowered partners in their care, supported by sophisticated AI tools and guided by compassionate, knowledgeable healthcare providers. This system will deliver better outcomes at lower costs while respecting patient autonomy and preserving the human elements that make healthcare meaningful.
Conclusion: Toward a More Informed Partnership
The Collaborative Care Framework represents more than just a new business model for primary care; it embodies a fundamental reimagining of the relationship between patients, healthcare providers, and medical knowledge. By harnessing the natural curiosity and research instincts of patients while providing clinical validation and safety oversight, this framework has the potential to transform healthcare delivery in ways that benefit all stakeholders.
The traditional model of healthcare, where patients passively receive care from authoritative providers, is increasingly incompatible with modern patient expectations and technological capabilities. Patients have unprecedented access to medical information and sophisticated AI tools that can help them understand their health conditions and treatment options. Rather than viewing this as a threat to medical authority, the framework embraces patient empowerment as a valuable resource that can enhance rather than undermine clinical care.
The economic implications of the framework are significant and far-reaching. By creating new revenue streams through technology subscriptions, care coordination services, and outcome-based payment arrangements, the framework offers a sustainable alternative to the traditional fee-for-service model that has contributed to physician burnout and patient dissatisfaction. The framework also creates opportunities for improved efficiency and reduced costs through better patient engagement and adherence to treatment recommendations.
The technology infrastructure supporting the framework demonstrates the potential for AI to enhance rather than replace human healthcare providers. AI systems excel at processing information, identifying patterns, and providing personalized education, while human providers bring clinical judgment, empathy, and complex decision-making capabilities that remain essential for effective healthcare delivery.
The clinical validation component of the framework ensures that patient empowerment does not compromise safety or quality of care. By providing systematic review and interpretation of patient research activities, the framework maintains clinical standards while enabling patients to become more informed and engaged partners in their care.
The early adopters of the framework demonstrate its potential across different healthcare settings and patient populations. From rural community health centers to urban specialty practices, the framework has shown the ability to improve patient outcomes, increase satisfaction, and create more sustainable practice models.
The challenges and limitations of the framework, including concerns about liability, health equity, and implementation complexity, are significant but not insurmountable. Addressing these challenges requires careful planning, comprehensive training, and ongoing support for both patients and providers. The framework must be implemented thoughtfully to ensure that it benefits all patients rather than exacerbating existing disparities in healthcare access and quality.
The future of healthcare will likely be characterized by increasing patient empowerment, sophisticated AI capabilities, and collaborative care models that leverage the strengths of both human and artificial intelligence. The Collaborative Care Framework provides a roadmap for this transformation, demonstrating how technology can be used to strengthen rather than replace the fundamental human relationships that make healthcare meaningful.
The success of the framework ultimately depends on the willingness of healthcare providers to embrace a new model of practice that values patient intelligence and curiosity while maintaining clinical expertise and safety standards. This requires a cultural shift in how healthcare providers view their roles and relationships with patients, moving from authoritative expertise toward collaborative partnership.
For health tech entrepreneurs, the framework represents a significant opportunity to create meaningful impact while building sustainable business models. The key is to focus on solutions that enhance the patient-provider relationship rather than circumventing it, creating value for all stakeholders while improving health outcomes.
The Collaborative Care Framework is not a destination but a journey toward a more informed, engaged, and effective healthcare system. As AI capabilities continue to advance and patient expectations evolve, the framework will need to adapt and evolve as well. The goal is not to create a perfect system but to establish a foundation for continuous improvement and innovation in healthcare delivery.
The ultimate measure of success for the framework will be its impact on patient outcomes, provider satisfaction, and healthcare costs. If the framework can demonstrate improvements in these areas while maintaining safety and quality standards, it will provide a compelling model for the future of healthcare delivery that can be scaled across different healthcare systems and patient populations.
The transformation envisioned by the Collaborative Care Framework extends beyond incremental improvements to existing healthcare delivery models. It represents a fundamental reimagining of how medical knowledge is shared, validated, and applied in clinical practice. By empowering patients to become active research partners while maintaining rigorous clinical oversight, the framework creates a new paradigm where the traditional boundaries between patient and provider become more fluid and collaborative.
The success of this model depends critically on the willingness of healthcare providers to embrace a new professional identity that values patient intelligence and curiosity as assets rather than obstacles. This requires a cultural shift away from the traditional medical hierarchy toward a more egalitarian approach where physicians serve as expert guides and validators rather than sole authorities on medical knowledge. For many physicians, this transition may feel uncomfortable initially, as it challenges deeply ingrained assumptions about professional roles and responsibilities.
However, early evidence suggests that physicians who embrace this collaborative approach often find it more professionally satisfying than traditional practice models. When patients arrive at appointments well-informed and prepared with relevant questions, clinical discussions become more sophisticated and meaningful. Physicians report feeling more intellectually engaged when they can focus on complex diagnostic reasoning and treatment planning rather than basic patient education and information gathering.
The framework also addresses one of the most significant sources of physician burnout by creating more efficient and productive patient encounters. When patients have conducted structured research under clinical guidance, appointment time can be devoted to interpretation, validation, and collaborative decision-making rather than explaining basic concepts or correcting misinformation from unreliable internet sources.
The economic sustainability of the framework requires careful attention to value creation for all stakeholders. Patients must perceive sufficient benefit from enhanced services and improved outcomes to justify any additional costs or time investments. Insurance companies and healthcare systems must see demonstrable improvements in cost-effectiveness and quality metrics to support coverage and implementation of framework services.
The most promising aspect of the framework is its potential to address healthcare disparities by democratizing access to high-quality medical information and education. Patients who previously lacked access to specialized medical knowledge due to geographic, economic, or social barriers can benefit from AI-powered research tools and community support networks. However, realizing this potential requires intentional design and implementation strategies that address digital literacy, language barriers, and other factors that might prevent equitable access.
The framework's emphasis on holistic treatment pathways alongside conventional medical interventions reflects a growing recognition that optimal health outcomes often require attention to lifestyle factors, social determinants of health, and patient preferences that extend beyond traditional medical interventions. By incorporating both evidence-based medical treatments and validated complementary approaches, the framework can address the whole person rather than just isolated symptoms or conditions.
As artificial intelligence capabilities continue to advance, the framework will likely evolve to incorporate even more sophisticated tools for patient education, symptom analysis, and treatment optimization. Machine learning algorithms will become better at personalizing recommendations based on individual patient characteristics, preferences, and response patterns. However, the core principle of human clinical validation and oversight will remain essential for maintaining safety and ensuring that technological capabilities enhance rather than replace human judgment and compassion.
The global implications of the framework are particularly significant for addressing healthcare challenges in resource-limited settings. AI-powered patient education and clinical validation tools can extend the reach of limited healthcare expertise, enabling patients in underserved regions to access sophisticated medical knowledge while maintaining appropriate clinical oversight through telemedicine and other remote consultation technologies.
The research opportunities created by the framework are substantial and could contribute significantly to medical knowledge and evidence-based practice improvement. The systematic collection and analysis of patient research patterns, treatment responses, and outcome data could provide valuable insights into disease progression, treatment effectiveness, and patient preferences that inform clinical guidelines and best practices.
Professional education and training will need to evolve significantly to prepare healthcare providers for this new model of collaborative practice. Medical schools and residency programs must incorporate training in patient education, shared decision-making, technology integration, and collaborative care approaches. Continuing education programs will help practicing physicians develop the skills and comfort level necessary to implement the framework effectively.
The regulatory environment will also need to adapt to address the unique challenges and opportunities created by AI-powered patient research and clinical validation systems. This will require ongoing dialogue between healthcare providers, technology developers, and regulatory agencies to ensure that innovations enhance patient safety and care quality while not creating unnecessary barriers to beneficial developments.
Looking toward the future, the Collaborative Care Framework represents just the beginning of a broader transformation in healthcare delivery that recognizes patients as intelligent partners capable of contributing meaningfully to their own care when provided with appropriate tools, education, and clinical support. This transformation has the potential to create a healthcare system that is more efficient, effective, and satisfying for both patients and providers while addressing many of the systemic challenges that currently plague primary care medicine.
The vision of empowered patients working collaboratively with engaged physicians, supported by sophisticated AI tools and validated through rigorous clinical processes, offers hope for addressing the crisis in primary care while creating new opportunities for innovation and improvement in healthcare delivery. The framework provides a roadmap for this transformation, demonstrating how technology can strengthen rather than replace the fundamental human relationships that make healthcare meaningful and effective.
The journey toward this new model of healthcare delivery will require sustained commitment, careful implementation, and ongoing refinement based on experience and outcomes. However, the potential benefits for patients, providers, and the healthcare system as a whole make this a transformation worth pursuing with energy, creativity, and determination. The future of healthcare depends not on choosing between human expertise and artificial intelligence, but on finding ways to combine them effectively in service of better health outcomes and more satisfying healthcare experiences for everyone involved.